The landscape of veterinary oncology has undergone a profound transformation, moving decisively away from rigid, one-size-fits-all protocols toward a highly personalized and client-centered strategy for managing canine lymphoma. This modern philosophy is built on a collaborative partnership between the veterinary team and the pet parent, with the central focus on clearly defining treatment goals that resonate with the family’s unique values, financial realities, and logistical capabilities. This entire process is methodically structured around answering three fundamental questions that form a logical roadmap for care: “What is it?” which drives the diagnostic phase; “Where is it?” which informs the staging process; and “How do we treat it?” which guides the development of a tailored therapeutic plan. This framework ensures every clinical decision is made with intention, compassion, and the pet’s best interest at the forefront, transforming a daunting diagnosis into a manageable journey.
The Diagnostic Journey Pinpointing the Enemy
Securing a Definitive Diagnosis
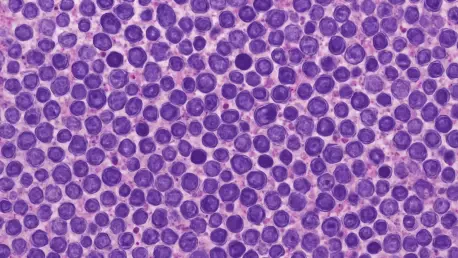
The initial step in addressing a potential lymphoma case, answering the question “What is it?”, almost invariably begins with a fine needle aspirate (FNA), a common and minimally invasive procedure. However, the success of this crucial first tool hinges on a key practical adjustment due to the nature of the cancer cells themselves. Lymphoma cells are notoriously delicate, described as being exceptionally “fragile, fragile cells,” a characteristic that frequently leads to ruptured cells and a frustrating “nondiagnostic” result from the pathology lab. To circumvent this common pitfall and avoid the difficult and anxious-making conversation with an owner about needing to repeat the procedure, the modern approach strongly advocates for an immediate in-house quality control step. This involves the simple act of staining and reviewing a single slide from the aspirate right after collection. This quick check confirms that a diagnostic sample, rich with intact cells, has been successfully obtained before the remaining slides are packaged and sent to an external pathologist for a definitive diagnosis.
This proactive measure is more than just a procedural tweak; it is a cornerstone of compassionate and efficient care that directly impacts the emotional well-being of the pet owner. Receiving an inconclusive result after an already stressful veterinary visit prolongs uncertainty and can erode confidence. By implementing this simple in-house review, veterinarians take control of the sample quality, significantly increasing the likelihood of a first-time diagnostic success. This practice underscores a shift toward prioritizing not just clinical accuracy but also the client experience. The cellular fragility of lymphoma means that routine handling can be enough to destroy the very evidence needed for a diagnosis. Understanding this cytological characteristic and adapting the collection process accordingly demonstrates a deeper, more nuanced approach to oncology that minimizes patient discomfort and provides anxious families with clear, actionable answers as swiftly as possible, setting a positive and trust-filled tone for the complex journey ahead.
Refining the Diagnosis With Advanced Techniques
Beyond simply identifying the presence of lymphoma, a critical refinement in the modern diagnostic process is the use of immunophenotyping to determine the cancer’s origin. This advanced technique distinguishes whether the lymphoma is composed of B-cells or T-cells, a distinction that is far from academic. This information is clinically vital as it directly influences the dog’s prognosis and is a primary driver in formulating the most effective treatment strategy. While traditional methods for this determination involved surgical biopsy followed by immunohistochemistry, the field has increasingly pivoted toward using flow cytometry on samples obtained via fine needle aspiration. This shift offers a less invasive option, but its success is contingent on proper sample handling, as the analysis requires a sufficient population of “live cells” to be accurate. As diagnostic technology continues to advance, even newer molecular tools, such as PCR for antigen receptor rearrangements (PARR), are becoming part of the expanding toolkit, offering an even deeper level of insight into the specific molecular characteristics of the cancer.
The prognostic weight carried by the B-cell versus T-cell distinction cannot be overstated, as it fundamentally alters the conversation between the veterinarian and the pet parent. Generally, B-cell lymphoma, which is the more common form, carries a more favorable prognosis and tends to be more responsive to the standard multi-agent chemotherapy protocols, such as CHOP. In contrast, T-cell lymphoma is often more aggressive, may be associated with paraneoplastic syndromes like hypercalcemia, and can be more resistant to conventional treatments, sometimes necessitating different or more intensive therapeutic approaches. Therefore, performing immunophenotyping is a non-negotiable step in modern veterinary oncology. It equips the clinical team and the family with crucial information needed for shared decision-making, allowing for a more accurate discussion about expected outcomes, the potential duration and intensity of treatment, and associated costs, perfectly aligning with the core philosophy of creating a personalized and transparent plan of care.
Strategic Staging Understanding the Battlefield
Intentional Testing for a Clearer Picture
Once a definitive diagnosis is confirmed, the clinical focus pivots to staging, the process of answering the critical question, “Where is it?” This step is essential for determining the extent of the disease throughout the dog’s body, which in turn provides invaluable prognostic information and serves as the foundation for a comprehensive treatment plan. A common and often surprising clinical paradox in canine lymphoma is that while many patients appear outwardly healthy and are classified as substage A (clinically well), the vast majority are diagnosed in an advanced stage of the disease, typically stage 3, 4, or 5. To navigate this complexity, experts now champion a philosophy of “intentional diagnostic testing” over the outdated practice of reflexively ordering a standardized “minimum database.” This thoughtful approach involves a meticulous scrutiny of basic laboratory work for subtle but significant indicators of systemic disease. For instance, the presence of hypercalcemia can be a paraneoplastic sign associated with certain types of lymphoma, while cytopenias, or low blood cell counts, may suggest that the cancer has infiltrated the bone marrow.
The practical application of this intentional staging strategy relies heavily on key imaging modalities that serve as the cornerstones for mapping the disease. The standard recommended tests include a full set of thoracic radiographs (chest x-rays) and a thorough abdominal ultrasound. These non-invasive tools provide a detailed view of the internal organs and lymph nodes, allowing the oncologist to assess for disease involvement beyond the initially identified peripheral lymph nodes. Chest x-rays are crucial for evaluating the sternal and mediastinal lymph nodes within the chest cavity, while a comprehensive abdominal ultrasound is relied upon to inspect for visceral involvement. The liver and spleen are frequently implicated in the later stages of lymphoma, and ultrasound can reveal changes in their size, texture, and architecture that are indicative of cancerous infiltration. This targeted use of imaging provides a clear, three-dimensional picture of the cancer’s spread, enabling a more accurate stage classification and, consequently, a more precise and effective treatment strategy.
Re-Evaluating Traditional Staging Components
A significant evolution in the modern approach to staging canine lymphoma involves the critical re-evaluation of once-routine procedures, most notably the bone marrow aspirate. Historically considered a standard component of a full staging workup, this invasive procedure is now understood to have limited utility in a large number of cases. The contemporary, evidence-based perspective asserts that after comprehensive thoracic and abdominal imaging have been performed, the addition of a bone marrow aspirate often “didn’t really change anything as far as staging.” In other words, the information gleaned from the bone marrow analysis rarely alters the fundamental understanding of the disease’s extent in a way that would change the recommended course of treatment. This realization that the procedure doesn’t significantly “move the needle much” in terms of the overall clinical picture represents a major shift away from dogmatic protocols and toward a more pragmatic and patient-centric approach.
The rationale behind this paradigm shift is rooted in clinical logic and a focus on therapeutic decision-making. If imaging has already confirmed that the lymphoma has spread to internal organs like the liver or spleen, the patient is already classified as having Stage IV or V disease. Confirming the presence of cancer cells in the bone marrow would also result in a Stage V classification, but it would not typically change the core treatment recommendation, which would be systemic chemotherapy regardless. The primary benefit of omitting the bone marrow aspirate when it is not clinically essential is multifaceted. It reduces the financial burden on the client, minimizes the stress, discomfort, and risks associated with sedation and the procedure itself for the patient, and contributes to a more streamlined and efficient diagnostic process. This calculated omission reflects a mature understanding of which diagnostic tests provide actionable information, ensuring that every step taken is purposeful and directly contributes to improving the patient’s outcome and quality of life.
The Art of Treatment and the Dawn of New Options
Tailoring Therapy to the Patient and Family
Addressing the final and most crucial question, “How do we treat it?”, is often described less as a science and more as an “art” that requires profound finesse and deep customization. The sheer variability in pet parent goals, patient health status, and logistical constraints necessitates a wide and flexible spectrum of therapeutic options. At one end of this spectrum lies the “gold standard” multi-agent chemotherapy protocol known as CHOP, an acronym for cyclophosphamide, doxorubicin, vincristine, and prednisone. While CHOP is highly effective and offers the best chance for a long-term remission, it also represents a major commitment of time, emotional energy, and financial resources for the family. At the other end are less aggressive single-agent chemotherapy regimens or purely palliative care, which may involve only prednisone to enhance comfort and quality of life without focusing on extending lifespan. Central to navigating this spectrum is a transparent, empathetic, and non-judgmental conversation with the client, reassuring them that “There’s no right or wrong here. The only answer here is what’s best for you and your family and your pet.”
To fully appreciate the therapeutic spectrum, it is helpful to understand the principles behind the different approaches. The CHOP protocol is considered the gold standard because its multi-agent design attacks cancer cells at different phases of their life cycle, a strategy that maximizes cell kill and helps overcome or prevent the development of drug resistance. Each component plays a distinct role: cyclophosphamide is an alkylating agent that damages cancer cell DNA, doxorubicin is an anthracycline antibiotic that interferes with DNA replication, vincristine is a vinca alkaloid that disrupts cell division, and prednisone is a corticosteroid that is directly toxic to lymphoid cells while also reducing inflammation and improving the patient’s sense of well-being. In stark contrast, a palliative approach forgoes these aggressive cytotoxic drugs entirely. The goal shifts from fighting the cancer to managing its symptoms. Using a drug like prednisone alone can shrink lymph nodes, stimulate appetite, and increase energy levels for a period, providing a good quality of life, albeit for a shorter duration. This comparison clearly illustrates the different paths available and underscores why the initial goal-setting conversation is the most important part of treatment planning.
A Glimpse into the Future of Therapeutics and Screening
The future of treatment is continuously being shaped by pharmaceutical innovation, with emerging therapeutics offering new hope and options. One such promising development is verdinexor, a conditionally licensed oral drug that introduces a novel mechanism of action. It is a selective inhibitor of nuclear transport, a process that cancer cells often hijack. By blocking a specific export protein, verdinexor effectively traps critical tumor suppressor proteins inside the cell’s nucleus, allowing them to perform their natural function of controlling cell growth and inducing the death of cancerous cells. Clinical data has shown an encouraging 37% overall response rate, and it may be particularly effective for the more challenging T-cell lymphomas. A significant advantage is that it does not appear to cause cross-resistance to other types of chemotherapy, making it a valuable tool that can be integrated into broader treatment plans. Furthermore, when addressing the universal client concern about treatment-related side effects, studies have indicated that it generally does not have a negative impact on a dog’s quality of life.
Beyond new treatments, the frontier of veterinary oncology is rapidly expanding toward proactive, non-invasive screening tools designed for early cancer detection. This addresses the frequent and hopeful question from clients: “Can’t you just do a blood test and tell me if my dog has cancer?” In response, novel blood-based screening platforms, often called liquid biopsies, are now a clinical reality. Initially developed to detect genomic signals associated with lymphoma, these tests are being expanded to cover over 50% of all common canine cancers. The primary goal of this technology is to shift the paradigm from diagnosing cancer after clinical signs appear to detecting it at a much earlier, subclinical stage when treatment is often more effective. A key performance metric for one such test is its extremely high specificity of 99%, making it highly accurate at ruling out the presence of disease. However, to maintain this accuracy and avoid misleading results, its use must be targeted to the appropriate screening population, generally recommended for dogs aged seven years and older or in at-risk breeds starting from the age of four. The integration of such early cancer screening into routine annual wellness protocols represents the future of proactive oncology care.
Redefining the Path Forward in Canine Oncology
The concerted evolution in veterinary medicine had fundamentally reshaped the approach to canine lymphoma. Through the integration of advanced diagnostics that offered deeper cellular insights, the adoption of highly personalized and flexible treatment plans, and the advent of emerging therapeutic and screening technologies, the journey of a lymphoma diagnosis was transformed. These advancements empowered veterinarians and pet owners alike, allowing them to navigate a once-daunting disease with greater clarity, confidence, and a broader array of options than had ever been available before. Ultimately, this modern, nuanced approach placed the highest priority not just on extending life, but on preserving the cherished bond and the quality of the life shared between a dog and its family.