Imagine a scenario where a patient presents with alarming neurological symptoms, and brain imaging reveals a large, tumor-like mass, sparking immediate concern for a life-threatening condition like cancer. This is the reality for individuals with Tumefactive Demyelinating Lesions (TDLs), a rare and often misunderstood variant of multiple sclerosis (MS) that mimics more sinister pathologies. Characterized by lesions larger than 2 cm, TDLs create diagnostic confusion due to their size, mass effect, and enhancement patterns on imaging, frequently leading to misdiagnosis as brain tumors or abscesses. This article delves into the intricacies of TDLs through a striking case study of a 46-year-old woman whose journey highlights the challenges of identifying and managing this condition. Coupled with an extensive review of medical literature, the discussion aims to illuminate the clinical, radiological, and therapeutic dimensions of TDLs. By weaving together real-world experience and scientific insights, the goal is to enhance understanding among healthcare professionals and underscore the importance of accurate recognition. The stakes are high, as missteps can result in unnecessary invasive procedures or delayed care. As the complexities of TDLs unfold, this exploration seeks to provide clarity on a condition that demands precision and awareness, particularly in environments where medical resources are scarce. Join in examining the diagnostic hurdles, cutting-edge tools, and evolving strategies that shape the management of this enigmatic disorder.
Unraveling the Diagnostic Puzzle
Tumefactive Demyelinating Lesions pose a significant challenge in clinical settings due to their uncanny resemblance to malignant brain tumors and other serious conditions like high-grade gliomas or primary central nervous system lymphomas. On imaging, these lesions often display a mass effect—pressure on surrounding brain tissue—and enhancement patterns that mimic cancerous growths, leading to frequent initial suspicions far removed from a demyelinating process. In the case of the 46-year-old woman central to this discussion, the first impression pointed toward a glioma, a misstep that echoes research findings indicating up to 30% of TDL cases face similar diagnostic uncertainty. Such errors can prompt invasive interventions like brain biopsies when less aggressive approaches might suffice. The overlap in presentation underscores why TDLs are a critical differential diagnosis for atypical brain lesions, especially in younger adults with a history of neurological symptoms. Avoiding misdiagnosis hinges on recognizing subtle clues that differentiate TDLs from neoplasms, a task that requires both advanced tools and a high index of suspicion among clinicians.
Compounding the diagnostic difficulty is the unreliability of standard tests like cerebrospinal fluid (CSF) analysis in confirming tumefactive demyelinating lesions (TDLs). Unlike classic multiple sclerosis, where markers such as oligoclonal bands often signal the disease, many TDL patients show inconclusive or normal CSF results, making diagnosis even more challenging. The featured patient exhibited no such markers over a 12-year period, aligning with studies that report these indicators are present in only 30-50% of cases. This inconsistency forces reliance on alternative diagnostic methods, as traditional tests fail to provide the clarity needed for swift and accurate conclusions. The risk of misdiagnosis carries heavy consequences, including inappropriate treatments or surgical procedures that could be avoided with better awareness. Emphasizing TDLs as a possible explanation for unusual brain lesions can steer care in the right direction, preventing delays and ensuring patients receive targeted interventions tailored to a demyelinating condition rather than a presumed malignancy.
Imaging Techniques as Diagnostic Cornerstones
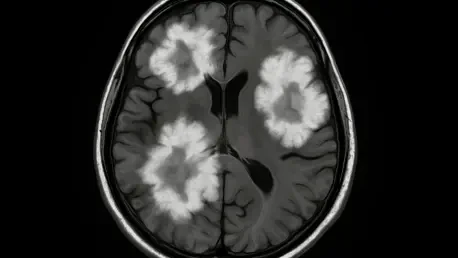
Magnetic Resonance Imaging (MRI) stands as the primary tool for detecting Tumefactive Demyelinating Lesions, though no single characteristic definitively identifies them, and understanding these nuances is critical for accurate diagnosis. Common findings include an incomplete or “open-ring” enhancement pattern after contrast administration, a relatively mild mass effect compared to the lesion’s size, and a tendency to spare the brain’s cortical gray matter. These traits help distinguish TDLs from tumors, which typically exhibit more pronounced mass effects and complete ring enhancement on scans. Understanding these radiological nuances is vital for narrowing down the differential diagnosis, particularly when clinical symptoms overlap with other neurological disorders. While MRI provides a foundational view, its limitations mean that additional methods are often necessary to build a comprehensive picture, especially in cases where the presentation is ambiguous or rapidly evolving.
Advanced imaging modalities, such as magnetic resonance spectroscopy (MRS) and perfusion-weighted imaging (PWI), offer deeper insights that enhance diagnostic precision for tumefactive demyelinating lesions (TDLs). In the case study under review, MRS revealed patterns indicative of demyelination rather than neoplasia, showing decreased N-acetylaspartate levels alongside elevated choline peaks. Similarly, PWI demonstrated reduced relative cerebral blood volume in the lesion area, a contrast to the elevated blood volume typical of tumors due to angiogenesis. These sophisticated techniques, while not universally accessible, provide critical data points that can tip the scales toward an accurate diagnosis. However, overlaps with other conditions persist, sometimes necessitating invasive procedures like biopsy when uncertainty remains. Combining multiple imaging approaches creates a more robust framework for identifying TDLs, reducing the likelihood of misclassification and ensuring that treatment aligns with the true nature of the condition.
Diverse Clinical Manifestations
The clinical presentation of Tumefactive Demyelinating Lesions varies widely, making them a diagnostic enigma that can appear as a standalone event, a precursor to relapsing-remitting multiple sclerosis (RRMS), or an atypical onset of aggressive disease. Symptoms often emerge acutely and are location-dependent, manifesting as hemiparesis, speech difficulties like aphasia, or even seizures. This diversity complicates initial assessments, as the signs can mimic stroke, infection, or malignancy depending on where the lesion resides in the brain. Recognizing the potential for TDLs amid such varied symptoms is essential for clinicians, as early suspicion can guide the diagnostic process toward appropriate testing rather than veering into unrelated treatment pathways. The unpredictable nature of these presentations demands a broad differential mindset to capture the full spectrum of possibilities.
In the highlighted case, the 46-year-old woman experienced a notably atypical trajectory, with episodes of optic neuritis occurring years before the emergence of a tumefactive lesion that triggered left-sided weakness and dysarthria. This 12-year latency between initial symptoms and the development of a significant lesion stands out as unusually prolonged, illustrating how the natural history of demyelinating disorders can defy conventional timelines. Research indicates that tumefactive demyelinating lesions (TDLs) predominantly affect younger adults, with a female predominance and peak incidence between the ages of 20 and 40. Approximately 25% of patients may progress to relapsing-remitting multiple sclerosis (RRMS) within five years, while others experience a monophasic course, highlighting the heterogeneous paths this condition can follow. Such variability necessitates individualized monitoring and care plans, ensuring that both immediate symptoms and potential future relapses are addressed with equal attention.
Histopathological Validation
When imaging and clinical evaluations leave diagnostic questions unanswered, a brain biopsy emerges as the gold standard for confirming Tumefactive Demyelinating Lesions (TDLs), providing definitive answers in complex cases. Histologically, these lesions typically reveal dense macrophage infiltration, perivascular lymphocytic inflammation, significant myelin loss with relative preservation of axons, and reactive astrocytic changes. These features sharply differentiate TDLs from neoplastic or infectious processes, providing clarity where non-invasive methods fall short. In the case of the 46-year-old patient, biopsy results confirmed a demyelinating pseudotumor, a critical finding that prevented the pursuit of aggressive oncologic treatments like surgical resection or radiation. This invasive step, though decisive, underscores the importance of exhausting less risky diagnostic avenues first, reserving biopsy for situations where uncertainty poses a greater threat than the procedure itself.
The reliance on histopathology, while effective, comes with inherent risks and is often considered a last resort in the diagnostic journey of TDLs. Complications such as infection, bleeding, or neurological impairment must be weighed against the need for definitive answers, particularly in cases where rapid progression heightens concern. The literature emphasizes that while biopsy offers unparalleled insight, advancements in non-invasive diagnostics are crucial to minimize its necessity. Efforts to refine imaging techniques and biomarkers aim to reduce the frequency of such procedures, ensuring that patients face fewer risks while still achieving diagnostic certainty. Until those innovations become widely available, histopathology remains an indispensable tool for resolving the most challenging TDL cases, guiding clinicians toward appropriate management strategies.
Therapeutic Approaches and Recovery
Managing Tumefactive Demyelinating Lesions often begins with high-dose intravenous corticosteroids, such as methylprednisolone, to address inflammation and reduce perilesional edema in the brain. This initial treatment proves effective for many patients, swiftly alleviating symptoms by curbing the immune response responsible for lesion formation. However, not all cases respond favorably, as seen in the experience of a 46-year-old woman whose condition resisted steroids, necessitating alternative interventions. The variability in response highlights the need for a flexible therapeutic arsenal, ready to adapt when first-line options fall short. Early intervention with corticosteroids can set the stage for recovery, but preparedness for resistance ensures that delays in effective treatment are minimized, preserving neurological function as much as possible.
For patients unresponsive to steroids, plasma exchange (PLEX) serves as a powerful second-line therapy, demonstrating efficacy in nearly 44% of severe central nervous system demyelination cases according to studies, and its impact can be transformative. In the featured case, PLEX resulted in marked clinical and radiological improvement, significantly reducing the lesion size and easing symptoms like weakness and speech impairment. Long-term management may involve disease-modifying therapies (DMTs) such as rituximab, natalizumab, or fingolimod, tailored to whether the condition presents as a one-time event or part of relapsing MS. The patient in question received rituximab for maintenance, reflecting a personalized approach to prevent future episodes. Timely and precise interventions can reverse inflammation and enhance outcomes, emphasizing that a stepped treatment strategy—moving from steroids to PLEX and DMTs as needed—plays a pivotal role in optimizing recovery for those with tumefactive demyelinating lesions (TDLs).
Barriers in Resource-Limited Environments
Diagnosing and treating Tumefactive Demyelinating Lesions in low-resource settings presents formidable challenges, largely due to restricted access to advanced diagnostic tools like MRI and specialized testing. In many regions, the absence of serial imaging or neuroimmunologic assays delays the recognition of TDLs, prolonging uncertainty and increasing the risk of misdiagnosis. The case study from Syria exemplifies these difficulties, as initial CSF and MRI results were inconclusive, and advanced diagnostics were not readily available, stretching the timeline to a confirmed diagnosis. Such systemic limitations highlight a critical gap in healthcare equity, where the inability to access cutting-edge technology can directly impact patient outcomes. Addressing these disparities requires innovative solutions that prioritize both accessibility and education to ensure timely identification of complex conditions like TDLs.
Beyond equipment shortages, low-resource environments often lack the interdisciplinary expertise needed to manage rare disorders effectively, creating significant challenges for healthcare providers. Neurologists, radiologists, and pathologists may not be readily available to collaborate, leaving local providers to navigate diagnostic ambiguities with limited support. This scarcity of specialized knowledge compounds the risk of errors, as seen in settings where prolonged diagnostic delays are common. The call for heightened awareness among healthcare workers in such areas is a recurring theme in the literature, advocating for training programs that focus on recognizing TDL symptoms and fostering connections with specialized centers. Practical steps like telemedicine consultations and international partnerships could bridge some of these gaps, ensuring that even in under-resourced regions, patients with TDLs receive care informed by the latest medical insights.
Epidemiological and Pathophysiological Insights
Tumefactive Demyelinating Lesions are exceedingly rare, accounting for just 0.1-0.3% of multiple sclerosis presentations, though this figure may be underestimated due to frequent misdiagnosis and limited access to diagnostic imaging in certain regions. Some research suggests a slightly higher prevalence in populations from Asia and Latin America, but data inconsistencies and reporting biases make definitive conclusions elusive. This scarcity of cases contributes to the general lack of familiarity among clinicians, often relegating TDLs to the periphery of differential diagnoses until more common conditions are ruled out. A deeper understanding of their epidemiology is essential for raising clinical suspicion, particularly in demographic groups or geographic areas where prevalence might be underreported, ensuring that TDLs are considered earlier in the diagnostic process.
Pathophysiologically, TDLs stand apart from typical MS lesions due to their confluent demyelination, pronounced macrophage activity, and a specific immune pattern often driven by antibodies and complement systems. Additional factors like oxidative stress and excitotoxicity may exacerbate lesion growth and the resulting mass effect, explaining why these lesions cause more significant disruption compared to smaller MS plaques. Ongoing research seeks to unravel the precise triggers and genetic predispositions that lead to this variant, aiming to identify why certain individuals develop tumefactive lesions while others follow a more classic MS trajectory. Such insights could inform future preventive measures or targeted therapies, shifting the approach from reactive treatment to proactive management. The complex interplay of immune mechanisms behind TDLs underscores the need for continued scientific exploration to refine both understanding and care.
The Power of Collaborative Care
Addressing Tumefactive Demyelinating Lesions effectively demands a multidisciplinary approach, uniting neurologists, radiologists, and pathologists to integrate clinical observations, imaging data, and laboratory results into a cohesive diagnosis. This collaborative framework proves indispensable when initial findings are ambiguous, as often occurs with TDLs due to their overlap with other neurological conditions. In the case of the 46-year-old patient, input from multiple specialists was crucial in shifting the suspicion from a brain tumor to a demyelinating lesion, preventing inappropriate interventions. Without such teamwork, the likelihood of diagnostic or therapeutic missteps increases, potentially compromising patient outcomes. A unified effort ensures that all facets of a case are examined, providing a comprehensive perspective that no single discipline could achieve alone.
The consensus within the medical community highlights the value of interdisciplinary collaboration, especially for rare and complex conditions like TDLs where expertise may not be centralized. Sharing knowledge across fields helps refine diagnostic criteria, standardize treatment protocols, and improve long-term management strategies. In settings where resources or specialists are limited, fostering these connections becomes even more critical, often requiring innovative solutions like virtual consultations or regional networks to access specialized input. The literature consistently advocates for building such collaborative systems, recognizing that integrated care not only enhances accuracy but also builds resilience in healthcare delivery. Ensuring that every patient benefits from a team-based approach remains a priority, particularly for disorders as diagnostically challenging as TDLs.
Moving Forward with Awareness and Action
Reflecting on the journey through the complexities of Tumefactive Demyelinating Lesions, it’s evident that past efforts in diagnosis and treatment have laid a critical foundation for better patient care, highlighting the importance of continued research and awareness. The case of the 46-year-old woman, whose prolonged diagnostic path eventually led to confirmation and effective management, mirrored the broader struggles documented in medical research to pinpoint this elusive condition. Historical challenges, from frequent misdiagnoses as brain tumors to delays in low-resource settings, underscored the urgency of raising clinical awareness. Each step taken, whether through biopsy confirmation or therapeutic interventions like plasma exchange, contributed to a growing body of knowledge that shaped how these rare lesions were understood and approached.
Looking ahead, the focus must shift to actionable strategies that build on these lessons, ensuring that the medical community is better equipped to handle challenges related to tumefactive demyelinating lesions (TDLs). Prioritizing education for healthcare providers worldwide can ensure TDLs are considered early in differential diagnoses, especially in cases of atypical brain lesions. Investment in accessible imaging technologies and telemedicine can help bridge resource gaps, bringing advanced diagnostics to underserved areas. Additionally, fostering global research collaborations could accelerate discoveries in pathophysiology and targeted therapies, offering hope for more precise interventions. Encouraging interdisciplinary teamwork remains essential to tackle diagnostic ambiguities and tailor treatments effectively. By committing to these steps, the medical community can transform past challenges into future successes, ensuring that patients with TDLs receive timely, accurate care regardless of where they are.