From Lifeline to Legal Battle: The High Stakes of the 340B Program
A critical financial support system designed to help safety-net healthcare providers serve America’s most vulnerable communities recently found itself at the center of an intense legal storm. The 340B Drug Pricing Program stands as a vital lifeline, allowing these hospitals and clinics to purchase outpatient drugs at steep discounts, which in turn enables them to stretch limited resources and maintain essential services. However, a contentious proposal by the Department of Health and Human Services (HHS) threatened to upend this long-standing system, sparking a fierce legal confrontation. This timeline traces the key events that led a federal court to issue a dramatic, last-minute injunction, temporarily halting a pilot program that would have fundamentally altered how these crucial discounts are administered. Understanding this conflict is essential, as it represents a major flashpoint in the ongoing national debate over the program’s purpose, integrity, and future.
From Proposal to Injunction: A Timeline of the Rebate Plan Conflict
The dispute escalated quickly over just a few months, culminating in a courtroom showdown that pitted the nation’s hospitals against the federal government. With each development, the stakes were raised, pushing the 340B program into a state of profound uncertainty.
Summer: The Rebate Pilot Program Is Unveiled
The conflict ignited when HHS announced a new pilot program designed to replace the 340B program’s traditional upfront discount model with a post-sale rebate system. For decades, eligible providers had purchased drugs directly at the discounted price, providing immediate savings and predictable cash flow. The new model, however, would have forced all 14,600 participating providers to pay the full price for drugs upfront. To recoup their savings, they would then have to submit complex data to manufacturers to claim a rebate later. This proposed shift from immediate savings to a delayed reimbursement model sent shockwaves through the healthcare community, which feared significant cash-flow problems and overwhelming new administrative burdens that could strain their already limited resources.
Mid-October: A Controversial Final Rule Accelerates Implementation
Despite widespread concerns from providers, HHS issued a final decision to proceed with the mandatory pilot, setting an aggressive launch date of January 1st. This decision gave hospitals just over two months to prepare for a seismic operational shift. The accelerated timeline became a central point of contention in the ensuing legal battle. Hospital groups argued passionately that this was an insufficient window to overhaul their complex procurement, billing, and data-tracking systems for some of the most commonly prescribed medications in the country, setting them up for financial and logistical failure.
December 1st: A Coalition of Hospitals Mounts a Legal Challenge
In response to the fast-approaching and non-negotiable deadline, a coalition led by the American Hospital Association (AHA) and other prominent hospital groups filed a lawsuit to block the pilot program. Their legal strategy centered on a powerful argument: that HHS had violated the Administrative Procedure Act (APA). They contended that the agency had illegally bypassed the required notice-and-comment rulemaking process, a cornerstone of transparent governance. Such a significant policy change, they argued, demanded a formal period for stakeholder feedback and a thorough agency review of its potential consequences—steps they insisted were unlawfully and deliberately skipped.
December 29th: A Federal Judge Halts the Program’s Launch
Just days before the pilot was set to begin, Judge Lance Walker of the Maine District Court granted the hospitals a preliminary injunction, effectively pausing the program. In a strongly worded ruling, Judge Walker labeled the pilot “hastily assembled” and agreed that providers would suffer “irreparable harm” from the loss of upfront discounts and the imposition of new administrative costs. He sharply criticized the government’s justification, pointing to a “threadbare administrative record” that suggested the agency failed to properly consider or justify the immense impact the rebate model would have on safety-net institutions. In a clear signal of the administration’s resolve, the Trump administration immediately filed an appeal, indicating its intent to continue fighting for the change.
The Injunction’s Impact and the Program’s Uncertain Future
The court’s injunction represents the most significant turning point in this conflict, shifting the immediate battle from implementation to litigation. The judge’s ruling hinged not on the merits of a rebate model itself but on the procedural failures of the government. This highlights a recurring pattern in which the Administrative Procedure Act serves as a crucial check on abrupt executive agency actions. While this legal pause provided immediate and welcome relief to hospitals, it has left the program’s long-term structure in limbo. The core conflict over discounts versus rebates remains unresolved, with the program’s future now depending on the outcome of the government’s appeal and the policy priorities of the new administration.
The Bigger Picture: Debating the Soul of the 340B Program
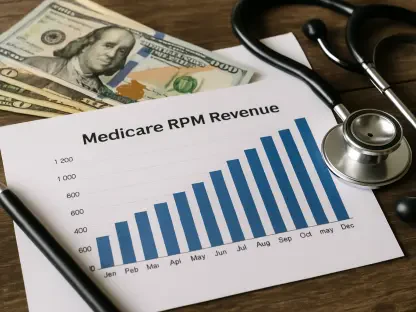
This legal drama is ultimately a symptom of a much larger, long-running debate over the soul of the 340B program. Proponents of the rebate model, including the pharmaceutical industry and government agencies, argue it is a necessary tool to enhance program integrity. They primarily cite concerns over “duplicate discounts,” a situation where a manufacturer provides both a 340B price and a separate Medicaid rebate for the same drug. These concerns are fueled by the program’s explosive growth, with purchases soaring from $43.9 billion to a record $66.3 billion in just two years. Critics like Senator Bill Cassidy argue the program has expanded beyond its original intent and that its financial benefits are not always passed on to patients. This view, however, overlooks a fundamental disagreement about the program’s core purpose. As Judge Walker noted in his ruling, hospitals rely on these savings “to stretch few resources as far as possible to serve rural and poor communities.” For them, the program is not a simple patient discount mechanism but a critical source of institutional funding that supports their entire safety-net mission. The court’s injunction has paused one battle, but the war over the program’s fundamental identity and future direction continues.