As we sit down with James Maitland, a renowned expert in public health policy and administration, we dive into the turbulent tenure of Robert F. Kennedy Jr. as HHS Secretary. With a career dedicated to understanding the intricacies of federal healthcare agencies like the Department of Health and Human Services (HHS) and the Centers for Disease Control and Prevention (CDC), James offers unparalleled insight into the controversies surrounding vaccine policy, leadership upheavals, and the broader implications for public health. Our conversation explores the widespread calls for Kennedy’s resignation, the internal chaos at the CDC, significant shifts in vaccine policy, and the impact of anti-science rhetoric on health policy decisions.
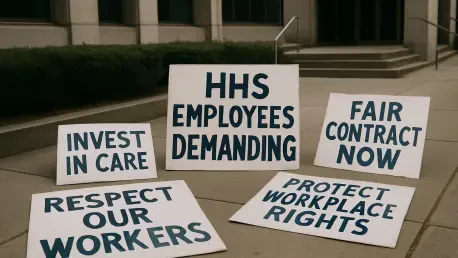
Can you explain what has prompted over 1,000 current and former HHS employees to demand Robert F. Kennedy Jr.’s resignation as Secretary?
The outcry from over 1,000 HHS employees stems from a deep concern that Kennedy’s leadership poses a direct threat to public health. Many of these employees, some of whom chose anonymity to avoid retaliation, believe his policies and actions are driven by personal biases rather than evidence-based science. They’ve accused him of destabilizing the department through mass firings and halting critical medical research grants, which they see as undermining the agency’s core mission. The sentiment is that his tenure is not just a bureaucratic issue—it’s a danger to the health of Americans across the board, regardless of political affiliation.
What specific policies or decisions under Kennedy’s leadership have fueled this strong backlash from HHS staff?
A major point of contention is Kennedy’s overhaul of vaccine policy. He dismissed members of the Advisory Committee on Immunization Practices, replacing them with individuals who either lack expertise in vaccines or are openly critical of them. Additionally, his decision to defund research into messenger RNA vaccines, which were pivotal during the COVID-19 response, has alarmed many within HHS. These moves, coupled with his history of anti-vaccine rhetoric, are seen as reckless and unscientific by staff who prioritize data-driven health strategies.
Can you describe the recent upheaval at the CDC and how it’s connected to Kennedy’s leadership?
The CDC has been in a state of crisis under Kennedy’s oversight. The firing of Director Susan Monarez, just a month after her Senate confirmation, was a bombshell. Her lawyer claims she was let go for refusing to endorse unscientific directives and for standing up against pressure to fire dedicated health experts. Following her departure, four senior CDC leaders also left, citing concerns about the direction of HHS. This cascade of exits has left the agency reeling, with morale at an all-time low and operations disrupted at a time when stability is crucial for public health responses.
How have Kennedy’s changes to vaccine policy at HHS unfolded, and what do they mean for the future?
Kennedy has made sweeping changes to vaccine policy that many see as alarming. Beyond replacing the Advisory Committee with less qualified or skeptical individuals, he’s also cut funding for messenger RNA vaccine research, which was a cornerstone of pandemic response. He’s even elevated voices that push discredited theories, like the notion that vaccines cause autism. These shifts could have long-term consequences, potentially eroding public trust in vaccines and weakening our ability to respond to future health crises. It’s a gamble that prioritizes ideology over science, and the ripple effects could be felt for years.
There’s been significant criticism of Kennedy’s response to the tragic shooting at the CDC headquarters in Atlanta. What can you tell us about this incident and the fallout?
The shooting on August 8 at the CDC headquarters in Atlanta, which resulted in the death of a police officer, was a heartbreaking event. Reports suggest the shooter’s motives were tied to anger and distrust over COVID vaccines, a sentiment some HHS staff believe has been fueled by political rhetoric—including Kennedy’s own statements—that vilifies public health workers. Staff are frustrated because they feel Kennedy has failed to adequately address their safety concerns or respond to their pleas for protection following the incident. This lack of action has only deepened the rift between him and the agency’s employees.
Given Kennedy’s history of anti-science rhetoric, particularly on vaccines, how has this influenced his decisions as HHS Secretary?
Kennedy’s long-standing skepticism of vaccines has clearly shaped his tenure. He’s made public comments over the years questioning vaccine safety and efficacy, often amplifying misinformation. As Secretary, this translates into policies like defunding critical research and reshaping advisory bodies to align with his views. Scientists and public health experts have reacted with dismay, arguing that his leadership undermines decades of progress in immunization and public health. His approach seems rooted in a personal crusade rather than the consensus of the scientific community.
Kennedy argues that his actions are aimed at restoring public trust in HHS. How do you see this playing out in reality?
Kennedy claims he’s rebuilding trust by eliminating corporate influence and bureaucratic inefficiency, pointing to changes like shaking up the Advisory Committee and pushing for reform at the CDC. However, his methods—firing thousands, sidelining experts, and ignoring evidence—seem to be having the opposite effect. Trust isn’t built by alienating your own workforce or disregarding science. Instead, we’re seeing growing distrust among both the public and health professionals, who worry that political agendas are trumping the agency’s mission to protect health. It’s a disconnect between his stated goals and the actual outcomes.
What is your forecast for the future of public health policy under this kind of leadership at HHS?
If this trajectory continues, I’m concerned we’re heading toward a significant erosion of public health infrastructure. Policies driven by skepticism of science rather than evidence could weaken our preparedness for future pandemics or outbreaks. Vaccine hesitancy might rise, undoing years of progress on preventable diseases. Morale at agencies like the CDC could further deteriorate, making it harder to attract and retain top talent. Without a shift toward evidence-based leadership, the long-term damage to public trust and health outcomes could be profound, and reversing it will take years, if not decades.