Welcome to an insightful conversation with James Maitland, a renowned expert in robotics and IoT applications in medicine, who brings a unique technological perspective to the pressing challenges in healthcare. With a deep passion for leveraging innovation to improve health outcomes, James offers valuable insights into the newly introduced $50 billion Rural Health Transformation Program. In this interview, we explore the origins and objectives of this ambitious initiative, the uncertainties surrounding its implementation, the distribution of funds, and the broader implications for rural healthcare providers and communities. Join us as we unpack how technology and policy intersect in addressing the critical needs of rural health systems.
Can you provide an overview of the Rural Health Transformation Program and explain what prompted its creation?
Absolutely. The Rural Health Transformation Program is a $50 billion initiative aimed at improving healthcare outcomes in rural areas over a five-year period starting in 2026. It was a last-minute addition to President Trump’s One Big Beautiful Bill Act, primarily as a compromise to secure votes from Republican lawmakers concerned about significant Medicaid cuts—projected at $155 billion over ten years. The core idea behind this fund is to offset some of those cuts by investing in rural health infrastructure and services, though there’s still a lot of debate about whether it will truly address the most urgent needs, especially for struggling hospitals.
What are some of the major uncertainties surrounding how this program will actually roll out?
There’s quite a bit of confusion right now, even among policy experts. The program was put together quickly, so the details on eligibility, specific goals, and how the funds will be prioritized are pretty vague. For instance, it’s unclear whether the focus is strictly on hospitals or broader health services. This lack of clarity creates a real challenge for states and healthcare providers trying to prepare applications or plan for the future. Without clear guidelines, there’s a risk of misaligned expectations or even wasted resources as entities guess at what CMS might approve.
How is the $50 billion funding structured, and what factors will influence its distribution across states?
The funding is split into two equal parts of $25 billion each. The first half will be distributed evenly among states with approved applications, which could disproportionately benefit states with fewer rural health challenges. The other half is allocated at the discretion of CMS Administrator Dr. Mehmet Oz, based on factors like the number of rural health centers in a state and more subjective assessments of hospital conditions. This discretionary power adds another layer of uncertainty, as it’s not entirely clear how those decisions will be made or prioritized.
States are required to submit detailed transformation plans to access these funds. Can you walk us through what these plans need to cover?
Sure. States must address eight specific elements in their transformation plans. Some are directly tied to the crisis facing rural hospitals, like identifying why so many are at risk of closure or reducing services, and improving access to hospital care. Others are broader, focusing on general health outcomes for rural residents, investing in new technology, and boosting clinician recruitment and retention. While some of these elements clearly target hospital sustainability, others could divert funds to different areas of rural health, which has sparked debate about where the money should really go.
There’s concern about the significant control CMS has over this program. How do you see this impacting states and their ability to use the funds effectively?
It’s a big issue. CMS decisions on funding allocations are nonreviewable, meaning states can’t appeal or challenge them, which limits their recourse if they disagree with the outcome. Additionally, if CMS believes a state isn’t using the funds as intended, it can withhold or reduce payments, or even claw back money already disbursed. This level of oversight could make states cautious or hesitant to propose innovative or unconventional uses of the funds, potentially stifling creative solutions to rural health challenges.
There’s a divide among experts on whether the funds should primarily support rural hospitals or other healthcare services. What’s your perspective on this debate, especially from a technology standpoint?
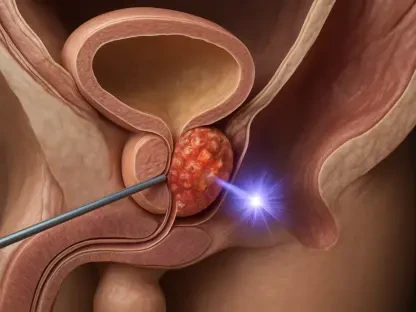
I think it’s a tough call, but there’s a strong case for prioritizing rural hospitals, especially the smaller ones at immediate risk of closure due to Medicaid cuts. These facilities are often the backbone of healthcare access in remote areas. However, from a tech perspective, I also see immense value in spreading funds to broader initiatives—like upgrading outdated IT systems or integrating IoT solutions for remote patient monitoring. These investments could create long-term efficiencies and improve care delivery across various settings, not just hospitals. The challenge is balancing immediate needs with sustainable innovation.
Looking ahead, what is your forecast for the future of rural healthcare given the temporary nature of this funding and the ongoing challenges?
I’m cautiously optimistic, but realistic. This $50 billion is a significant injection of resources, but it’s a one-time deal over five years, and the structural issues—like financial losses at half of rural hospitals and looming Medicaid cuts—aren’t going away. My forecast is that while this program might delay some closures and fund critical tech upgrades, it’s not a permanent fix. We need to pair this with longer-term strategies, like shifting to value-based care models or reforming Medicare Advantage to reduce payment delays. If we don’t, rural communities will continue to face declining access, and that’s a loss for everyone—patients, providers, and the vitality of these areas. I hope we see policymakers and tech innovators collaborate more deeply to build sustainable solutions beyond 2030.