A profound and largely unseen revolution is reshaping personal health management, driven not by a breakthrough in medicine but by the generative artificial intelligence now accessible on billions of personal devices. This evolution marks a significant pivot in AI’s role within healthcare, moving it from a specialized background tool used exclusively by clinicians and researchers to a frontline resource deployed directly by patients. The scale of this consumer-led adoption is staggering, revealing a deep-seated need among individuals to better understand and control their healthcare journeys. This is not a story about replacing doctors with algorithms for self-diagnosis. Instead, it is about the rise of an AI-powered companion that helps patients decode complex medical information, prepare for clinical encounters, and, most critically, contend with the immense administrative and financial labyrinths that characterize modern healthcare systems. This shift is empowering individuals to become more active and informed participants in their own well-being.
Bridging the Information and Accessibility Gap
The sheer volume of patient engagement with AI for health purposes highlights a critical gap in traditional care delivery. Globally, more than 40 million health-related prompts are entered into leading AI platforms like ChatGPT every day, a testament to the public’s search for accessible information. A revealing pattern in this usage is its timing, with approximately 70% of these conversations occurring outside of standard clinic hours. This positions AI as a crucial, always-available resource for individuals seeking guidance when their primary care provider is unreachable. This trend is particularly impactful in geographically isolated and underserved areas, including rural communities and “hospital deserts” where access to medical facilities and specialists is severely limited. While artificial intelligence cannot replace a closed hospital, it serves a vital upstream function by helping residents interpret symptoms, organize their health information, and make more educated decisions about when and where to seek formal medical attention, potentially optimizing patient engagement with a strained healthcare system.
Beyond providing medical information, AI has rapidly become an indispensable tool for navigating the daunting administrative challenges of healthcare, particularly in the United States. Millions of queries each week are dedicated to deciphering the complexities of health insurance, a clear indicator that consumers are independently leveraging technology to overcome systemic hurdles. Patients are using AI to perform detailed comparisons of insurance plans, understand labyrinthine pricing structures, and get clear explanations of benefits and coverage limits. Furthermore, they are using these tools to manage the often-frustrating processes of submitting claims, appealing denials, and clarifying ambiguous billing statements. By translating dense industry jargon into plain language and structuring complex financial information, AI is effectively demystifying the opaque business of healthcare. This allows individuals to tackle administrative burdens that previously seemed insurmountable without specialized knowledge, fostering a new level of consumer autonomy and financial literacy in healthcare.
The Rise of the AI-Assisted Patient Advocate
One of the most transformative applications of patient-facing AI is in the realm of self-advocacy, where it helps to rebalance the historical information asymmetry between patients and the healthcare system. Individuals are now equipped with a powerful tool to understand, question, and actively participate in their own care plans. A striking example of this empowerment involves patients successfully appealing denied insurance claims by using AI to locate and summarize supporting peer-reviewed medical literature, presenting a case that is difficult for insurers to dismiss. This same principle applies to clinical management, with patients using AI to track and visualize their lab results over time, helping them identify trends or ask more pointed questions during appointments. Others use it as a safety net, cross-referencing new prescriptions with their current medications to flag potential adverse interactions. This technology is lowering the barrier to entry for deep medical understanding, turning passive recipients of care into proactive partners in their own health.
This patient-driven movement is occurring in parallel with growing AI adoption among medical professionals, though for distinctly different purposes. A majority of physicians in the United States now utilize AI, but their focus is primarily on alleviating administrative burdens rather than on core diagnostics. Clinicians are leveraging these tools for tasks such as automating clinical documentation, generating summaries of lengthy patient records, and streamlining communication workflows. This allows them to reclaim valuable time that can be redirected toward direct patient care. This dual adoption—by both consumers and providers—illustrates that AI is not a single, monolithic solution but a versatile and distributed ecosystem. While physicians use it to enhance efficiency and combat burnout, patients use it to gain clarity and agency. Together, these complementary trends are fostering a more informed, efficient, and collaborative healthcare environment where technology supports both sides of the clinical relationship.
Redefining the Flow of Healthcare Information
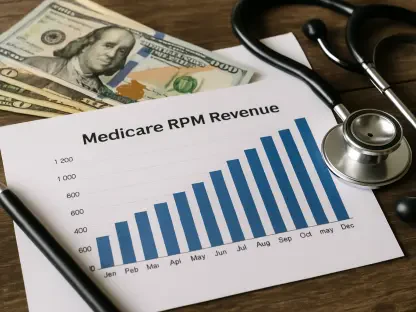
The widespread adoption of AI directly by patients ultimately marked a fundamental departure from the traditional, top-down models of healthcare. It became evident that this technology was no longer a tool confined to institutional settings but had transformed into a distributed and democratized ecosystem that fundamentally altered how information and decisions flowed through the entire system. This profound shift had significant and lasting implications, influencing everything from the design of patient engagement strategies to new considerations for future reimbursement models. Healthcare providers increasingly encountered patients who arrived at appointments not only better informed but also equipped with sophisticated data and analysis to actively co-pilot their own care. The established dynamic, which had long been characterized by a one-way transfer of knowledge from the expert to the recipient, had irrevocably given way to a more interactive, collaborative, and ultimately more effective healthcare paradigm.