Imagine a healthcare landscape where slashing operational costs doesn’t come at the expense of patient safety, and where sustainability transforms from a lofty ideal into a measurable impact. Reprocessed medical devices are turning this vision into reality, providing an innovative solution that balances affordability with environmental responsibility. These devices, previously used, undergo meticulous cleaning, sterilization, and refurbishment to meet rigorous safety standards, ensuring they perform just as reliably as brand-new instruments. Far from a fringe concept, this approach is gaining traction as a cornerstone of modern healthcare, addressing both financial constraints and ecological concerns with remarkable efficiency.
The numbers behind this trend are striking, highlighting a remarkable growth trajectory for the sector. With a market value of USD 3.3 billion in 2024, the industry is on a steep upward path, projected to reach USD 17.76 billion by 2035, driven by an impressive annual growth rate of 16.55%. This rapid expansion signals a growing recognition of the dual benefits these devices offer—cost savings for strained healthcare budgets and a significant reduction in medical waste. Hospitals and clinics adopting this model can redirect funds to critical areas like patient services or staff development, all while contributing to a greener planet. However, challenges such as professional skepticism and regulatory complexities persist, underscoring the need for education and robust oversight to ensure broader acceptance. As technology advances and emerging markets open up, the potential for reprocessed devices to redefine healthcare delivery continues to grow.
Economic Benefits of Reprocessed Devices
Cost Savings for Healthcare Providers
The financial advantages of integrating reprocessed medical devices into healthcare systems are profound and far-reaching, offering significant savings and resource reallocation opportunities. By choosing to reuse instruments that have been carefully sterilized and refurbished, hospitals and surgical centers can dramatically lower their procurement expenses. This reduction in costs is particularly vital at a time when healthcare expenditures are climbing relentlessly, placing immense pressure on budgets. Facilities can save substantial amounts on items like cardiovascular catheters or surgical tools, allowing them to allocate resources to other pressing needs, such as advanced diagnostic equipment or enhanced patient care programs. This shift not only eases financial burdens but also maintains the high standards of treatment that patients expect, proving that cost efficiency and quality are not mutually exclusive.
Beyond the immediate savings, the adoption of reprocessed devices fosters a more strategic approach to resource management within healthcare institutions. When procurement costs are reduced, administrators gain the flexibility to invest in long-term initiatives, such as staff training or infrastructure upgrades, which ultimately improve operational efficiency. This financial breathing room can be a game-changer for smaller clinics or underfunded hospitals that often struggle to balance quality care with limited funds. Moreover, the ripple effect of these savings can extend to patients, potentially reducing out-of-pocket costs for treatments. The economic model of reprocessing thus supports a more resilient healthcare system, capable of adapting to fiscal challenges without compromising on essential services.
Budget Allocation and Systemic Impact
Another dimension of the economic benefit lies in how reprocessed devices enable better budget allocation across healthcare systems, allowing facilities to make the most of their financial resources. With reduced spending on single-use instruments, facilities can prioritize investments in areas that directly enhance patient outcomes, such as hiring specialized personnel or expanding access to cutting-edge therapies. This reallocation is especially crucial in regions with high medical costs, where every dollar saved can make a tangible difference in the scope of care provided. The ability to stretch budgets further without sacrificing safety or efficacy positions reprocessed devices as a practical tool for systemic improvement.
Additionally, the cost-saving potential of these devices can influence broader healthcare policies and insurance frameworks. As more providers adopt reprocessing, there’s an opportunity to negotiate better reimbursement rates or develop funding models that reward sustainable practices. This could lead to a more equitable distribution of resources, particularly benefiting underserved communities that rely on public health systems. The economic ripple effects are clear—by cutting costs at the procurement level, the entire healthcare ecosystem stands to gain, fostering a cycle of reinvestment and innovation that strengthens the industry as a whole. This financial strategy underscores the transformative power of reprocessed devices in building a more sustainable economic foundation for healthcare delivery.
Environmental Impact and Sustainability
Reducing Medical Waste
The environmental case for reprocessed medical devices is as compelling as the economic one, addressing a critical issue in healthcare: the staggering volume of waste generated by single-use products. Every year, hospitals discard millions of disposable instruments, contributing to overflowing landfills and straining natural resources through constant production. Reprocessing offers a direct countermeasure by extending the lifecycle of these tools, significantly cutting down on waste. A single reprocessed device, reused multiple times under strict safety protocols, can prevent numerous equivalents from ending up as trash, aligning the healthcare sector with global sustainability goals and promoting a circular economy where resources are conserved.
This reduction in waste has broader implications for environmental stewardship within the industry, and by minimizing the need for new manufacturing, reprocessed devices also lower the carbon footprint associated with producing and transporting medical equipment. Hospitals adopting this practice can position themselves as leaders in eco-friendly operations, appealing to environmentally conscious stakeholders and meeting regulatory pressures for greener practices. The impact is not just local—less waste and reduced production demands contribute to global efforts to combat pollution and resource depletion. As more facilities embrace this model, the cumulative effect could reshape how healthcare interacts with the planet, turning a historically wasteful sector into a model of responsible consumption.
Aligning with Global Green Initiatives
Reprocessed medical devices also play a pivotal role in aligning healthcare with international sustainability initiatives. Many countries and organizations are pushing for reduced environmental impact across industries, and healthcare, being a significant contributor to waste, is under scrutiny to adopt greener practices. By integrating reprocessed instruments, providers can demonstrate compliance with these initiatives, supporting policies aimed at reducing industrial waste and promoting recycling. This alignment not only enhances the reputation of healthcare institutions but also positions them as active participants in a global movement toward sustainability.
Furthermore, the environmental benefits of reprocessing can influence patient and community perceptions, fostering trust in healthcare systems that prioritize ecological responsibility. As awareness of climate issues grows, patients are increasingly likely to support providers who adopt sustainable practices, creating a competitive edge for facilities that embrace reprocessed devices. This trend also encourages collaboration between healthcare providers and environmental organizations, potentially leading to innovative solutions for waste management. The synergy between reprocessing and green initiatives highlights how healthcare can contribute to a healthier planet, proving that clinical excellence and environmental care can go hand in hand in shaping a more sustainable future.
Technological Innovations Driving Safety
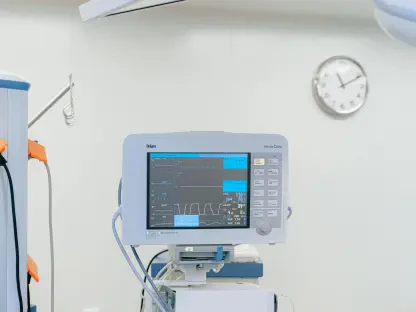
Advancements in Sterilization and Tracking
Technology stands as a cornerstone in ensuring the safety and reliability of reprocessed medical devices, addressing one of the most significant barriers to their adoption. Sophisticated sterilization methods, such as ethylene oxide and plasma techniques, have revolutionized the reprocessing industry by guaranteeing that devices are free from contaminants before reuse. These cutting-edge processes meet stringent safety standards, ensuring that reprocessed instruments perform on par with new ones. Additionally, digital tracking systems enhance transparency by monitoring the lifecycle of each device, from usage to reprocessing, providing a clear record of compliance and maintenance that builds confidence among healthcare providers.
Equally important is the role of innovation in overcoming operational challenges tied to reprocessed devices, which are becoming increasingly vital in modern healthcare. Digital inventory management systems streamline the tracking process, reducing the risk of errors and ensuring that only properly certified devices are reused. These systems also facilitate regulatory compliance by maintaining detailed logs, which are critical during audits or inspections. The integration of such technology not only boosts efficiency but also addresses lingering concerns about device reliability, offering concrete evidence of safety protocols. As these advancements continue to evolve, they pave the way for greater acceptance, demonstrating that reprocessed devices are a viable and secure option for modern healthcare settings.
Building Trust Through Innovation
The impact of technological progress extends beyond functionality to the critical realm of trust-building within the healthcare community. Advanced sterilization and tracking tools provide tangible proof that reprocessed devices meet the highest safety standards, directly countering skepticism among medical professionals. For instance, real-time data from digital systems can show the sterilization history of a device, reassuring clinicians of its readiness for use. This transparency is essential in shifting perceptions, as it offers a clear, evidence-based argument for the reliability of reprocessed instruments in clinical environments.
Moreover, ongoing innovation in this space signals a commitment to continuous improvement, which resonates with healthcare stakeholders. Research and development efforts focused on enhancing sterilization techniques or integrating artificial intelligence for predictive maintenance are already showing promise in further elevating safety standards. These forward-thinking approaches not only address current concerns but also anticipate future challenges, ensuring that reprocessed devices remain a trusted component of healthcare delivery. By leveraging technology to bridge the trust gap, the industry is steadily moving toward a future where reprocessed instruments are viewed as a standard, rather than an exception, in medical practice.
Challenges in Market Adoption
Professional Skepticism and Regulatory Complexity
Despite the clear benefits of reprocessed medical devices, significant hurdles remain in achieving widespread adoption, with professional skepticism topping the list of challenges. Many healthcare workers harbor reservations about the safety and effectiveness of reused instruments, even when advanced sterilization processes are in place. Misconceptions about potential contamination or performance issues can deter clinicians from embracing this option, creating a cultural barrier that slows market growth. Addressing these concerns requires targeted education campaigns to highlight the rigorous safety protocols and real-world success stories that demonstrate the reliability of reprocessed tools in clinical settings.
Regulatory complexity adds another layer of difficulty to the adoption process, making it challenging for companies to navigate the diverse landscape of requirements. Standards for reprocessing vary widely across regions, creating a patchwork of rules that companies must follow to ensure compliance. In some areas, overly stringent regulations can delay market entry, while in others, lax oversight raises concerns about quality control. Liability issues further complicate the landscape—if a reprocessed device fails, determining accountability can be contentious, deterring some facilities from taking the risk. Harmonizing regulations and establishing clear guidelines for responsibility are essential steps to streamline adoption and foster confidence among providers, ensuring that safety remains the top priority.
Overcoming Barriers with Education and Policy
Tackling professional skepticism and regulatory challenges demands a multifaceted approach, with education playing a central role. Training programs that detail the reprocessing journey—from collection to sterilization to reuse—can demystify the process for healthcare staff, dispelling myths and building trust. Real-world case studies showing successful outcomes with reprocessed devices can further reinforce their value, offering concrete evidence to counter doubts. Such initiatives, supported by industry leaders and regulatory bodies, are crucial for shifting mindsets and encouraging broader acceptance across diverse medical settings.
On the policy front, creating a more cohesive regulatory framework is vital to easing market entry and ensuring consistent quality, while also fostering trust among stakeholders in the healthcare industry. International collaboration to standardize reprocessing guidelines could simplify compliance for companies operating across borders, reducing operational friction. Additionally, clear policies on liability, perhaps through shared responsibility models between reprocessors and healthcare providers, can mitigate risks and encourage adoption. These combined efforts—education to change perceptions and policy reform to address operational challenges—offer a pathway to overcoming the barriers that currently hinder the full potential of reprocessed medical devices in transforming healthcare delivery.
Opportunities for Growth and Expansion
Emerging Markets and Third-Party Services
The future of reprocessed medical devices shines brightly with untapped potential, particularly in emerging markets where healthcare budgets are often constrained. Regions with limited resources see these devices as a lifeline, providing access to high-quality medical tools at a fraction of the cost of new ones. This affordability can expand care capabilities in underserved areas, addressing critical gaps in healthcare access while supporting economic development. As demand grows in these markets, companies have a unique opportunity to tailor solutions to local needs, fostering partnerships that drive both innovation and market penetration.
Third-party reprocessing services are another key avenue for growth, simplifying adoption for facilities lacking the infrastructure to handle reprocessing internally. These specialized firms manage the complex logistics of sterilization, testing, and certification, ensuring compliance with safety standards while allowing hospitals to focus on patient care. For smaller clinics or rural providers, this model removes the burden of investing in reprocessing equipment and training, making the transition to reused devices seamless. The rise of such services not only broadens market reach but also enhances operational efficiency, positioning reprocessed devices as a scalable solution across diverse healthcare environments.
Collaborative Innovation and Market Expansion
Collaboration stands as a powerful driver for expanding the reach and impact of reprocessed medical devices. Partnerships between manufacturers, reprocessing companies, and healthcare providers can spur innovation in device design, making instruments more suitable for multiple uses without compromising safety. Joint efforts to develop standardized reprocessing protocols can also streamline operations, reducing costs and improving accessibility. These collaborative initiatives are particularly impactful in emerging markets, where tailored solutions can address unique challenges like limited infrastructure or regulatory immaturity.
Furthermore, market expansion is fueled by growing awareness of sustainability as a priority in healthcare. As environmental concerns gain prominence, providers are increasingly motivated to adopt practices that reduce waste, creating a natural demand for reprocessed devices. Industry stakeholders can capitalize on this trend by advocating for policies that incentivize sustainable practices, such as tax benefits or grants for facilities that integrate reprocessing. By aligning with global sustainability goals and fostering innovation through collaboration, the market for reprocessed devices is poised to grow exponentially, offering a blueprint for a more responsible and inclusive healthcare system worldwide.
Regional Dynamics and Market Leadership
North America’s Dominance
North America emerges as the undisputed leader in the market for reprocessed medical devices, propelled by substantial healthcare investments and a robust regulatory framework. The region’s high medical expenditure creates a fertile ground for adopting cost-saving measures like reprocessing, while guidelines from agencies such as the FDA ensure that safety and quality remain paramount. Early adoption of advanced technologies, including digital tracking and cutting-edge sterilization methods, further solidifies North America’s position, enabling seamless integration of reprocessed devices into clinical workflows. This leadership sets a benchmark for other regions striving to balance cost efficiency with patient care standards.
Additionally, North America’s commitment to sustainability amplifies its market dominance, as hospitals and clinics in the region are increasingly aligning with eco-friendly practices, driven by both public demand and regulatory incentives. Partnerships with third-party reprocessors enhance operational efficiency, allowing facilities to scale up reprocessing efforts without significant internal investment. This collaborative ecosystem, combined with a strong focus on innovation, ensures that North America not only leads in market share but also in shaping global trends. The region’s success story serves as a model, demonstrating how strategic investments and regulatory support can drive the adoption of sustainable healthcare solutions.
Global Variations and Growth Potential
While North America leads, other regions like Europe and Asia Pacific are carving their own paths in the reprocessed medical devices market, shaped by unique local dynamics. Europe, with its strong emphasis on environmental regulations, is witnessing steady growth as healthcare systems prioritize waste reduction. However, varying national standards can slow adoption, requiring harmonized policies to unlock full potential. Meanwhile, Asia Pacific offers immense growth opportunities due to its large, cost-sensitive markets, though underdeveloped infrastructure and regulatory frameworks pose challenges that demand tailored approaches for successful market entry.
The diversity in regional adoption highlights the need for customized strategies to maximize growth potential globally. In Europe, aligning reprocessing practices with stringent environmental mandates can accelerate acceptance, while in the Asia-Pacific region, investments in infrastructure and training can bridge existing gaps. Collaborative efforts between global companies and local stakeholders are essential to navigate these variations, ensuring that reprocessed devices meet regional needs while maintaining universal safety standards. As these areas continue to develop their capabilities, the global market stands to benefit from a more interconnected and inclusive approach, driving the circular healthcare economy to new heights through shared innovation and adaptation.
Reflecting on a Sustainable Path Forward
Looking back, the journey of reprocessed medical devices revealed a transformative shift in healthcare, where economic savings and environmental responsibility converged to address pressing industry challenges. The market, which stood at USD 3.3 billion in 2024, embarked on a path toward USD 17.76 billion by 2035, underpinned by a remarkable growth rate. Technological strides in sterilization and tracking tackled safety concerns head-on, while North America’s leadership showcased the power of regulatory support and innovation in driving adoption. Challenges like skepticism and regulatory hurdles were met with persistent efforts to educate and standardize, paving the way for broader acceptance.
Moving forward, the focus must shift to actionable strategies that sustain this momentum and ensure long-term success in the healthcare sector. Stakeholders should prioritize global collaboration to harmonize regulations, ensuring consistent quality across borders. Investment in education programs for healthcare professionals can further erode doubts, while incentives for adopting sustainable practices could accelerate uptake in hesitant regions. Emerging markets, with their unique needs, deserve tailored solutions to enhance access to affordable care. By fostering partnerships and leveraging technology, the industry can build on past achievements to create a resilient healthcare system—one that values resource conservation as much as patient outcomes, ensuring a balanced and sustainable future for all.