A groundbreaking shift is underway in oncology, as a new class of treatment leverages molecular precision to seek and destroy cancer cells from within the body, marking a significant departure from conventional therapeutic strategies. A recent gathering of leading experts in oncology and nuclear medicine has crystallized the consensus that Radiopharmaceutical Therapies (RPT) are establishing a new frontier in the fight against cancer. The rapid clinical adoption and profound potential of these treatments, particularly agents like Lutetium-177 (Lu-177) PSMA-617 for advanced prostate cancer, were central to the discussions. These conversations have solidified a view of RPT as a highly effective and transformative approach, while simultaneously bringing into focus the operational, educational, and regulatory challenges that must be navigated to unlock its full potential. The fundamental advantage of these therapies rests in their elegant mechanism, which uses systemically administered radioactive isotopes attached to targeting molecules that act as biological guides, delivering a lethal dose of radiation directly to tumors while sparing healthy tissue.
The Clinical Evidence and Impact
Validating a New Standard of Care
The clinical validation of this targeted methodology was powerfully demonstrated through a pivotal meta-analysis presented by leading researchers. This comprehensive review aggregated data from seven randomized phase II and III clinical trials, which collectively involved a robust cohort of more than 2,500 patients diagnosed with metastatic castration-resistant prostate cancer (mCRPC). The results provided unequivocal evidence that patients treated with Lu-177 PSMA-617 experienced a statistically significant prolongation of progression-free survival (PFS) when compared to those receiving the current standard-of-care systemic treatments, which predominantly include androgen receptor signaling inhibitors. This finding signifies a crucial advancement, offering patients a therapeutic option that can more effectively control the disease’s advancement and delay the onset of further symptoms or complications, thereby improving their quality of life during a critical phase of their illness. The strength of this evidence has created a compelling argument for the reevaluation of current treatment protocols for advanced prostate cancer.
Crucially, this significant extension of disease control was not achieved at the cost of increased patient hardship, a common trade-off with many potent cancer therapies. The analysis reinforced the favorable tolerability of Lu-177 PSMA-617, confirming that its use did not correspond with an increase in grade 3 or higher toxicities. While a statistically significant difference in overall survival was not demonstrated, this outcome was largely attributed to the confounding effects of crossover trial designs, where patients in the control arms were subsequently permitted to receive the radiopharmaceutical therapy after their disease progressed. This design element, while ethically sound, complicates the assessment of long-term survival benefits. Nevertheless, the compelling PFS data, combined with the manageable safety profile, has fostered a strong consensus among oncologists that RPT should be integrated much earlier into the management algorithms for patients with advanced prostate cancer, rather than being reserved as a last-resort option.
Building the Infrastructure for a New Modality
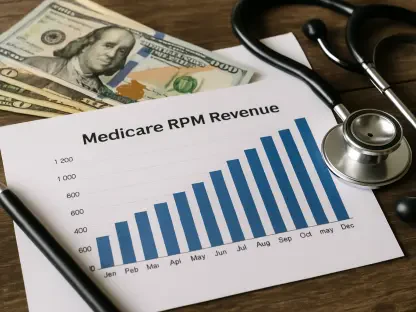
The demonstrated clinical success of RPT is fueling an unprecedented surge in its real-world application, a trend confirmed by national healthcare utilization data. Analysis of Medicare claims reveals that the administration of these advanced therapies has increased by more than 20-fold over the past decade, from 2016 to 2026. This exponential growth is not isolated within a single specialty but spans a wide range of medical fields, including diagnostic and interventional radiology, nuclear medicine, radiation oncology, and medical oncology/hematology. Current practice patterns indicate that radiologists are administering the majority of these therapies, highlighting an evolving clinical landscape that demands enhanced collaboration and standardized protocols across different disciplines. This rapid uptake underscores the urgent need to establish a robust infrastructure capable of supporting the widespread and safe delivery of radiopharmaceuticals, ensuring that the quality of care keeps pace with the escalating demand from a growing patient population.
Consequently, a significant focus of recent expert discussions has been on addressing the operational challenges inherent in establishing and sustaining high-quality RPT programs. Evidence-based frameworks were presented to create cohesive clinical workflows adaptable to diverse healthcare settings, from smaller community practices to large academic medical centers. These frameworks consistently emphasize the critical importance of a dedicated, multidisciplinary team. Such a team must encompass the specialized expertise of nuclear medicine professionals for proper radiopharmaceutical handling and dosimetry, radiation oncologists for oversight of radiation delivery and safety protocols, and medical oncologists for comprehensive patient management and the strategic integration of RPT with other systemic therapies. The recent promulgation of consensus guidelines and white papers by organizations such as the American Society for Radiation Oncology (ASTRO) provides a foundational resource, offering detailed guidance on quality assurance and radiation safety protocols specifically tailored to the unique requirements of this new treatment modality.
Educating the Next Generation and Pioneering the Future
Meeting the Demand for Specialized Expertise
The explosive adoption of radiopharmaceutical therapies has created an acute and immediate need for a larger workforce of physicians and support staff who are proficient in the unique complexities of this treatment modality. The successful implementation of RPT requires a deep understanding of radiobiology, nuclear medicine principles, radiation safety, and patient-specific dosimetry, a skill set that transcends traditional oncologic training. This knowledge gap presents a significant bottleneck to expanding patient access and ensuring the safe, effective administration of these powerful agents. Addressing this shortage is not merely a matter of increasing numbers but of developing a new cadre of specialists who can confidently manage every aspect of the RPT process, from initial patient selection and treatment planning to long-term follow-up and management of potential side effects. The long-term success and scalability of RPT are therefore directly dependent on a concerted effort to build this specialized workforce from the ground up.
In response to this pressing challenge, ASTRO has launched a major educational initiative designed to establish a network of national training centers dedicated to radiopharmaceutical therapy. These centers are being developed to provide rigorous, standardized training and credentialing for physicians in all facets of RPT. The comprehensive curriculum will cover appropriate patient selection criteria, accurate dosimetry calculations to optimize therapeutic effect while minimizing toxicity, safe handling and administration of radioactive materials, and the navigation of the complex regulatory landscape governing these treatments. This proactive effort is considered essential to guaranteeing that the rapid expansion of RPT access does not inadvertently compromise patient safety or treatment efficacy. By creating a clear pathway for physicians to gain and demonstrate proficiency, this initiative aims to set a national standard for care, ensuring that patients receive the highest quality treatment regardless of where they are treated.
The Evolving Landscape of Treatment and Innovation
The future of radiopharmaceutical therapy will be shaped by the intricate interplay between scientific innovation, stringent regulatory oversight, and dynamic commercial development. Discussions led by influential figures, including former high-ranking FDA officials, have highlighted the complex journey from laboratory discovery to clinical availability. This process requires continuous and transparent collaboration among academic researchers, pharmaceutical companies, and regulatory bodies to streamline the development and approval of new agents. Furthermore, the burgeoning portfolio of next-generation radiopharmaceutical agents currently under investigation promises to significantly broaden the applicability of this therapeutic approach. Researchers are actively exploring novel molecular targets that will extend the use of RPT to a wider range of malignancies, including hematologic cancers, gastrointestinal tumors, and other solid tumors that have historically been difficult to treat, ushering in a new era of personalized cancer medicine.
Among the most exciting frontiers in this field is the development of agents that employ alpha-particle emitters. These radioisotopes deliver a more potent and highly localized form of radiation compared to the beta emitters currently in wide use. The high energy and short path length of alpha particles result in dense, complex, and highly lethal double-stranded DNA breaks within tumor cells, offering the tantalizing prospect of enhanced tumor-killing power while further minimizing collateral damage to surrounding healthy tissue. The path forward involves a multi-pronged strategy focused on optimizing the sequencing and combination of RPT with other treatment modalities, such as immunotherapy and chemotherapy, as demonstrated in innovative combination trials like the phase II LUNAR study. The field’s progress has hinged on harmonizing multidisciplinary collaboration to navigate persistent regulatory and reimbursement hurdles, which has ensured broad and equitable patient access to these transformative therapies.