In the ever-evolving landscape of cancer treatment, radiopharmaceutical therapy (RPT) emerges as a groundbreaking precision medicine approach, delivering targeted radiation directly to cancer cells to minimize damage to surrounding healthy tissue. This innovative method holds immense promise for improving patient outcomes, yet it also presents significant challenges due to the complexity of its administration and the potential risks involved. A recent publication by the Society of Nuclear Medicine and Molecular Imaging (SNMMI) in The Journal of Nuclear Medicine underscores that the key to maximizing RPT’s potential lies in robust multidisciplinary collaboration. By uniting experts from diverse fields such as nuclear medicine, oncology, and medical physics, this collaborative approach ensures safer and more effective therapy delivery. The emphasis on teamwork addresses critical gaps in expertise and standardization, paving the way for enhanced treatment quality. As RPT continues to gain traction, the integration of varied professional skills becomes not just beneficial, but essential for navigating its intricacies and achieving the best results for patients battling cancer.
Harnessing Diverse Expertise for RPT Success
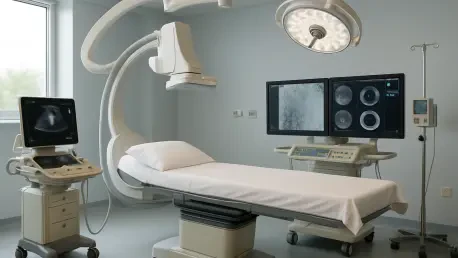
The implementation of radiopharmaceutical therapy demands a high level of precision, as even minor errors in radiation delivery can have serious consequences for patient safety and treatment efficacy. Multidisciplinary collaboration stands as a vital strategy to mitigate these risks, bringing together nuclear medicine physicians, medical physicists, radiopharmacists, and oncologists to form a cohesive unit. Each professional contributes unique insights, from evaluating a patient’s medical history to ensuring accurate dosimetry, creating a comprehensive framework for care. This team-based dynamic allows for thorough patient assessments, ensuring that treatment plans are tailored to individual needs while addressing potential complications before they arise. The synergy of such diverse expertise not only enhances the technical aspects of RPT but also fosters a deeper understanding of how to balance therapeutic benefits with safety considerations, ultimately leading to improved outcomes in cancer management.
Beyond the technical execution, multidisciplinary teams play a crucial role in fostering a patient-centered approach within RPT delivery. By integrating perspectives from various healthcare domains, these teams ensure that decisions are made through shared processes, taking into account the full spectrum of a patient’s condition and preferences. For instance, oncologists provide critical context about cancer progression, while nuclear medicine specialists focus on the optimal use of radiopharmaceuticals. This collaborative dialogue helps in crafting personalized treatment strategies that prioritize both effectiveness and patient well-being. Additionally, the involvement of support staff, such as nurses and patient educators, ensures that individuals undergoing RPT are well-informed and supported throughout their journey. Such a holistic approach minimizes oversight and builds trust, reinforcing the importance of teamwork in addressing the multifaceted challenges posed by advanced cancer therapies like RPT.
Establishing Standards Through Unified Efforts
Standardization remains a cornerstone for ensuring the safety and consistency of radiopharmaceutical therapy across diverse healthcare settings, and multidisciplinary collaboration is key to achieving this goal. By adhering to strict quality management programs mandated by the Nuclear Regulatory Commission (NRC), teams of experts work together to develop and implement protocols that reduce variability in treatment delivery. Medical physicists, for instance, ensure that equipment calibration meets precise standards, while nuclear medicine professionals oversee the correct administration of radiopharmaceuticals. This joint effort helps to eliminate errors that could compromise patient safety, creating a reliable framework for RPT application. The commitment to uniform practices, driven by interdisciplinary input, underscores the importance of accountability in maintaining high-quality care for cancer patients undergoing this complex therapy.
Further emphasizing the push for standardization, initiatives like the SNMMI’s Radiopharmaceutical Centers for Excellence Program exemplify how collaborative frameworks can set benchmarks for excellence. These programs, supported by partnerships with entities such as the International Accreditation Commission (IAC), rely on the combined expertise of various professionals to establish rigorous safety and quality criteria for RPT facilities. The collaborative nature of these initiatives ensures that standards are not only developed but also effectively implemented across different regions and institutions. By fostering a culture of continuous improvement, multidisciplinary teams help to address discrepancies in practice, ensuring that every patient receives treatment that meets the highest possible standards. This unified approach to quality control is essential for building confidence in RPT as a safe and effective cancer treatment option, highlighting the transformative power of teamwork in healthcare innovation.
Advancing Skills and Global Reach Through Collaboration
Education forms a critical pillar in the advancement of radiopharmaceutical therapy, and multidisciplinary collaboration significantly enriches the learning environment for professionals in this field. The SNMMI provides an array of educational resources, including annual conferences, specialized webinars, and training events focused on theranostics and RPT. These platforms bring together experts from nuclear medicine, oncology, and related disciplines to share knowledge and best practices, ensuring a well-rounded curriculum that addresses both clinical and technical challenges. By facilitating interactions among diverse professionals, these programs equip practitioners with the latest skills needed to handle the complexities of RPT administration. This collaborative educational effort not only enhances individual competence but also builds a robust workforce capable of pushing the boundaries of cancer treatment through informed and innovative practices.
On a broader scale, the drive for international harmonization of RPT guidelines reflects the global dimension of multidisciplinary collaboration. Through partnerships with organizations like the International Atomic Energy Agency (IAEA) and the European Association of Nuclear Medicine (EANM), the SNMMI works to align standards and practices worldwide, reducing disparities in access to this cutting-edge therapy. Teams of experts from various countries and specialties contribute to creating unified protocols that ensure consistent quality and safety in RPT delivery, regardless of geographic location. This cross-border cooperation addresses unique regional challenges while promoting equitable access to advanced cancer treatments. By fostering a shared commitment to excellence, such global teamwork ensures that the benefits of RPT reach patients everywhere, demonstrating how collaborative efforts can transcend boundaries to improve health outcomes on an international level.
Reflecting on Collaborative Milestones
Looking back, the strides made in radiopharmaceutical therapy underscore the profound impact of multidisciplinary collaboration on cancer care. Teams of dedicated professionals from nuclear medicine, oncology, and physics united to tackle the intricate challenges of RPT, ensuring safer and more effective treatments through shared expertise. Initiatives driven by the SNMMI, alongside partnerships with global bodies, laid down standardized protocols that enhanced consistency and patient safety across various settings. Educational programs and international outreach further solidified a foundation of knowledge and equitable access, reflecting a collective resolve to advance this precision medicine approach. Moving forward, sustaining this momentum through continued teamwork and innovation will be crucial. Strengthening interdisciplinary networks and investing in training can address remaining gaps, while expanding global cooperation promises to bring RPT benefits to even more patients, shaping a future where cancer treatment is both precise and universally accessible.