In the high-stakes world of healthcare, laboratory errors pose a silent threat to patient safety, often leading to misdiagnoses, delayed treatments, and eroded trust in medical systems, making their prevention a critical priority for hospitals. These mistakes, whether from a mislabeled specimen or a faulty test result, can have cascading effects on clinical decisions that impact lives. With lab results forming the backbone of modern diagnostics, ensuring their accuracy is not merely an option but an absolute imperative for hospitals. The challenge lies in identifying the root causes of these errors, which often span human oversight, systemic flaws, and technological gaps. This article delves into actionable strategies that healthcare institutions can implement to minimize diagnostic inaccuracies. By exploring the phases of errors, the role of human factors, and the power of technology and culture, a comprehensive approach to prevention emerges. The goal is clear: to transform laboratories into bastions of reliability where precision underpins every patient outcome.
Unpacking the Nature of Diagnostic Mistakes
Laboratory errors infiltrate every stage of the diagnostic process, manifesting in pre-analytical, analytical, and post-analytical phases with distinct yet interconnected challenges. Pre-analytical errors often arise before testing begins, stemming from mishandled samples, incorrect labeling, or improper storage conditions that compromise data integrity. Analytical errors occur during testing, frequently due to malfunctioning equipment or deviations from standard procedures that skew results. Post-analytical errors, meanwhile, emerge after testing, when results are misinterpreted or inaccurately reported to clinicians. Understanding these phases is critical for hospitals aiming to design targeted interventions. Without a clear grasp of where breakdowns occur, efforts to improve accuracy remain superficial at best. Mapping out these error zones allows for a strategic focus on prevention, ensuring that each segment of the diagnostic chain receives the attention it demands to safeguard patient care from avoidable mistakes.
Beyond the procedural stages, the human element plays a pivotal role in the prevalence of laboratory errors, often acting as both the source and potential solution to diagnostic mishaps. Staff may inadvertently mislabel specimens under time pressure or fail to follow protocols due to inadequate training, leading to results that misguide treatment plans. Fatigue, high workloads, and lack of familiarity with updated guidelines further exacerbate these risks, turning minor oversights into major consequences. Hospitals must recognize that even the most dedicated professionals are susceptible to error in demanding environments. Addressing this requires a shift in perspective—viewing human mistakes not as isolated failures but as symptoms of broader systemic gaps. By prioritizing the human factor, institutions can develop strategies that empower staff to perform with greater precision, ultimately reducing the likelihood of errors that jeopardize patient safety and trust in healthcare delivery.
Creating Strong Frameworks for Error Reduction
One of the most effective ways hospitals can curb laboratory errors is by investing in continuous training and robust oversight mechanisms to elevate staff competency and accountability. Regular workshops, simulation exercises, and refresher courses ensure that lab technicians remain well-versed in the latest protocols, from sample collection to result interpretation. Beyond education, implementing strict procedural checks, such as mandatory double-verification of specimen labels, can intercept errors before they escalate into diagnostic failures. Hospitals should also establish mentorship programs where seasoned professionals guide newer staff, fostering a culture of learning rather than blame. This approach not only sharpens technical skills but also builds confidence among team members to adhere to best practices under pressure. By embedding training and oversight into daily operations, healthcare facilities lay a solid foundation for minimizing human-induced errors and enhancing the reliability of lab outcomes.
Standardization of processes across all laboratory functions serves as another critical pillar in the fight against diagnostic inaccuracies, creating consistency where variability often breeds mistakes. Developing uniform protocols for sample handling, testing procedures, and result reporting eliminates ambiguity, ensuring that every task is performed predictably regardless of the personnel involved. Hospitals must periodically review these guidelines to incorporate advancements in medical standards and address emerging risks. For instance, creating checklists for high-risk steps like specimen transport can prevent lapses that lead to compromised samples. Standardization also facilitates smoother communication between departments, reducing the chance of errors during handoffs. When every staff member operates under the same set of rules, the likelihood of procedural deviations diminishes significantly. This systematic alignment transforms laboratories into more cohesive units, where precision becomes the norm rather than the exception in diagnostic workflows.
Harnessing Technology to Boost Precision
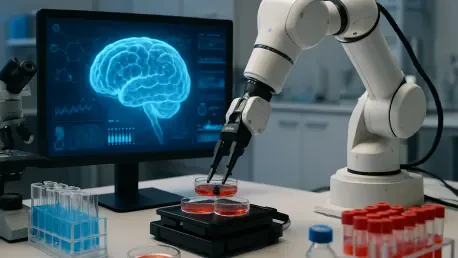
The integration of cutting-edge technology offers hospitals a powerful arsenal to combat laboratory errors, significantly enhancing accuracy through automation and intelligent systems. Barcode tracking for specimens, for example, virtually eradicates mislabeling by replacing manual identification with error-proof digital tagging. Similarly, artificial intelligence platforms can analyze test results, flagging anomalies for human review and acting as a safeguard against oversight. These tools reduce the burden on staff, allowing them to focus on complex tasks while minimizing repetitive errors. Hospitals adopting such innovations must ensure seamless integration into existing workflows to maximize their impact. As technology evolves, staying ahead of the curve with these solutions becomes essential for maintaining diagnostic integrity. The shift toward tech-driven labs signals a future where human limitations are offset by digital precision, paving the way for safer patient care.
Equally important is the commitment to regular maintenance and auditing of laboratory equipment and systems, as technological failures can undermine even the best error-prevention strategies. Routine calibration of machines ensures that test results remain accurate, while scheduled maintenance prevents unexpected breakdowns that disrupt workflows. Hospitals should also conduct comprehensive audits of their tech infrastructure to identify vulnerabilities, such as outdated software or hardware prone to glitches. These proactive measures help catch potential issues before they manifest as diagnostic errors affecting patient outcomes. Establishing partnerships with equipment manufacturers for timely updates and repairs can further bolster reliability. By treating technology not as a static tool but as a dynamic asset requiring constant care, healthcare institutions can uphold the highest standards of accuracy. This diligence ensures that the technological backbone of laboratories remains robust, supporting error-free diagnostics in every test conducted.
Cultivating a Culture of Responsibility
Creating an environment of transparent error reporting stands as a cornerstone for hospitals aiming to address and prevent laboratory mistakes systematically. When staff feel safe to disclose errors or near-misses without fear of punishment, institutions gain valuable insights into recurring issues and their root causes. This openness enables swift corrective actions, such as revising protocols or providing targeted training, before small lapses escalate into serious harm. Hospitals can facilitate this by implementing anonymous reporting systems and emphasizing that the goal is improvement, not blame. Leadership must actively demonstrate support for such transparency, ensuring that reported errors lead to constructive dialogue rather than repercussions. A culture built on trust and honesty allows for continuous learning, turning mistakes into opportunities to strengthen diagnostic processes. This shift in mindset is vital for uncovering hidden flaws and fostering a shared commitment to patient safety across all levels of the organization.
Collaboration across departments further amplifies error prevention by aligning laboratory teams with clinicians, administrators, and other stakeholders in a unified mission for accuracy. Regular interdisciplinary meetings can bridge communication gaps, ensuring that lab results are understood and acted upon correctly by those making treatment decisions. Joint training sessions also help build mutual understanding of each team’s role in the diagnostic chain, preempting misunderstandings that could lead to errors. For instance, clinicians can provide feedback on result clarity, while lab staff can highlight challenges in sample collection from clinical settings. Hospitals should encourage such interactions as a standard practice, breaking down silos that often hinder effective error management. By fostering a collective approach, institutions ensure that preventing laboratory mistakes becomes a shared responsibility, not a burden shouldered by one department alone. This synergy enhances overall care quality, reinforcing trust in diagnostic outcomes.
Reflecting on Steps Forward for Safer Diagnostics
Looking back, the journey to mitigate laboratory errors revealed a multifaceted challenge that hospitals tackled through systemic reforms, technological advancements, and cultural shifts. Training programs were refined to address human oversight, while standardized protocols curbed procedural inconsistencies that once plagued diagnostics. Technology, from barcode systems to AI-driven analysis, emerged as a game-changer, offering precision where manual efforts faltered. Transparent reporting and interdisciplinary collaboration also played pivotal roles, ensuring that errors were learned from rather than hidden. Moving forward, hospitals must sustain this momentum by regularly evaluating the effectiveness of these strategies and adapting to new challenges. Investing in emerging tools and fostering global knowledge-sharing can further elevate standards. The path ahead lies in an unwavering dedication to innovation and accountability, ensuring that laboratories evolve into trusted pillars of healthcare where patient safety remains paramount.