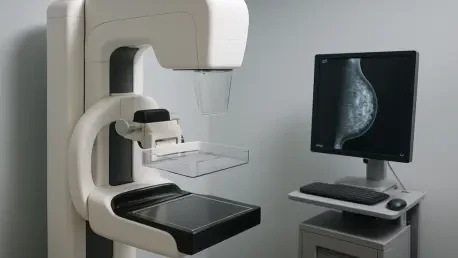
For countless women, the challenge of dense breast tissue has cast a shadow over the reliability of traditional breast cancer screening, often hiding tumors in plain sight on standard mammograms and leaving nearly half of those screened vulnerable to undetected malignancies. This persistent barrier, which complicates early diagnosis and heightens cancer risk, has driven researchers to explore innovative imaging solutions that could transform outcomes. A pivotal study, the Density MATTERS trial, recently published in Radiology, unveils a promising dual approach using Molecular Breast Imaging (MBI) and Digital Breast Tomosynthesis (DBT). Conducted across leading medical centers like the Mayo Clinic and MD Anderson, this trial involved nearly 3,000 asymptomatic women with dense breasts over five years, testing whether combining these advanced technologies could significantly enhance the detection of invasive cancers. The results suggest a potential paradigm shift, raising the question of whether this strategy might redefine screening standards for a population long underserved by conventional methods.
Unraveling the Dense Breast Dilemma
Dense breast tissue presents a formidable obstacle in breast cancer screening, as it often appears indistinguishable from tumors on X-ray-based imaging, including both traditional mammography and the more advanced DBT. While DBT offers a step forward with its 3D, multi-angle images compared to older 2D methods, its sensitivity still falters in dense breasts, frequently resulting in missed diagnoses. This limitation is particularly alarming given that nearly half of women undergoing screening have dense tissue, which not only masks potential cancers but also elevates their inherent risk of developing the disease. The consequences of these missed opportunities for early detection can be dire, with tumors often progressing to later, less treatable stages before discovery. Addressing this gap has become a critical priority in medical imaging, pushing the boundaries of technology to ensure that no cancer remains hidden due to anatomical challenges. The urgency of this issue sets the stage for exploring novel approaches that can penetrate the veil of density and deliver accurate, life-saving results.
The Density MATTERS trial emerges as a beacon of hope in tackling the dense breast challenge, focusing on a population that conventional screening often fails. By enrolling women aged 40 to 75 with confirmed dense tissue across diverse clinical settings, the study ensures its findings are relevant to a broad demographic. The trial’s design, spanning multiple years and involving rigorous follow-ups, underscores the depth of commitment to understanding how imaging limitations can be overcome. Dense breasts increase cancer risk by creating a complex imaging environment where structural similarities obscure critical abnormalities, often delaying diagnosis until symptoms appear. This delay can mean the difference between manageable treatment and advanced disease, highlighting the need for tools that go beyond surface-level imaging. As the trial’s outcomes begin to reshape perspectives, they emphasize that solving this diagnostic puzzle requires rethinking the very foundation of how breast cancer is detected in high-risk groups.
Harnessing the Dual Strength of MBI and DBT
Molecular Breast Imaging (MBI) introduces a transformative angle to breast cancer screening by focusing on metabolic activity rather than just physical structure, a stark contrast to the capabilities of DBT. While DBT excels at providing detailed 3D images of breast tissue, it often struggles in dense environments, missing subtle or early-stage tumors. MBI, a nuclear medicine technique, uses a radiotracer to pinpoint areas of abnormal cellular behavior, revealing cancers that structural imaging might overlook. In the Density MATTERS trial, MBI identified 30 cancers in 29 participants that DBT alone could not detect, with a significant 71% classified as invasive and often caught at an early stage. This ability to uncover hidden malignancies marks MBI as a critical complement to existing methods, addressing a gap that has long frustrated clinicians. The trial’s data suggest that relying solely on structural imaging is no longer sufficient for comprehensive screening in dense breast cases, pointing toward a more integrated diagnostic future.
The true power of the Density MATTERS trial lies in the synergy between MBI and DBT, which together create a robust screening strategy far surpassing the capabilities of either technology alone. When combined, these modalities significantly increased the detection rate of invasive breast cancers, often identifying them before they spread to lymph nodes—a crucial factor in improving patient prognosis. Notably, the dual approach detected all node-positive cases in the first year of screening, compared to only 57% by DBT independently, demonstrating its potential to prevent progression to advanced stages. This combined strength not only boosts the number of cancers found but also ensures they are caught at more treatable points, potentially reducing the need for aggressive interventions. Such findings highlight how blending structural and functional imaging can address the shortcomings of traditional methods, offering a more complete picture of breast health. This partnership between technologies could herald a new standard, ensuring fewer cancers slip through the cracks in dense breast screening.
Prioritizing Patient Safety and Accessibility
Beyond its diagnostic prowess, the adoption of MBI alongside DBT brings notable patient-centered advantages that make it a viable option for widespread use in supplemental screening. The radiotracer used in MBI boasts a well-established safety profile, borrowed from cardiac imaging, and triggers fewer adverse reactions compared to alternatives like contrast-enhanced mammography or MRI. This reduced risk profile is vital for ensuring that women feel comfortable undergoing additional imaging without fear of significant side effects. Additionally, the moderate cost of MBI positions it as a practical choice, especially when compared to more expensive modalities that may not be accessible to all. For women with dense breasts, who often require more than standard screening, this balance of safety and affordability is a game-changer. The trial’s emphasis on these practical benefits suggests that integrating MBI into routine care could remove barriers to advanced diagnostics, making enhanced screening a reality for diverse populations.
Accessibility and equity also play a central role in the potential rollout of MBI and DBT as a combined screening tool, as evidenced by the trial’s diverse participant pool. With 12% minority enrollment and testing conducted across both academic centers and community hospitals, the study addresses concerns about whether such innovations can benefit a wide range of women, regardless of socioeconomic or geographic factors. This inclusivity strengthens the case for adopting this dual approach on a larger scale, ensuring that advancements in breast cancer detection do not remain confined to privileged settings. Patient tolerance for the procedure, coupled with its manageable cost, further supports the argument for integrating this method into standard protocols for dense breast screening. By focusing on real-world applicability, the trial lays the groundwork for a future where advanced imaging is not a luxury but a standard option, bridging gaps in healthcare disparities and prioritizing patient well-being alongside diagnostic accuracy.
Shaping the Future of Tailored Breast Cancer Detection
The Density MATTERS trial reflects a broader movement toward personalized breast cancer screening, recognizing that a one-size-fits-all approach falls short, especially for women with dense breasts. The integration of DBT’s structural precision with MBI’s functional insights represents a shift in radiology and oncology toward customizing protocols based on individual risk factors and anatomical challenges. This tailored strategy maximizes diagnostic accuracy by ensuring that the unique needs of each patient are met, rather than relying on a single imaging method that may fail in specific contexts. The trial’s success in detecting early-stage, invasive cancers—often at a median size of just 0.9 centimeters—underscores the value of this precision, as catching malignancies before they progress can drastically improve survival rates. Such findings advocate for a future where screening is not a uniform process but a carefully calibrated one, designed to address the specific barriers posed by conditions like dense breast tissue.
Looking ahead, the trial’s implications extend beyond immediate clinical practice to inspire further innovation in breast cancer care, focusing on early intervention as a cornerstone of reducing mortality. The emphasis on identifying node-negative cancers through MBI highlights how critical it is to detect disease at its most treatable stage, potentially sparing patients from the burdens of advanced treatments. This aligns with the overarching goal of modern oncology to shift the focus from reaction to prevention, using technology to outpace cancer’s progression. Future research sparked by these results may explore optimal screening intervals, integration with other emerging tools, and long-term impacts on survival rates. Additionally, real-world studies on cost-effectiveness and patient acceptance will be essential to scaling this dual-modality approach across diverse healthcare systems. The vision of personalized screening, where each woman receives a strategy suited to her unique profile, moves closer to reality with every step forward from trials like this one.
Reflecting on a Milestone in Screening Innovation
Looking back, the Density MATTERS trial marked a turning point in addressing the diagnostic challenges of dense breast tissue, demonstrating that the combined use of MBI and DBT significantly enhanced the detection of invasive cancers. This dual approach uncovered malignancies that standard imaging missed, often at early, treatable stages, and set a new benchmark for what comprehensive screening could achieve. The trial’s commitment to diversity and practical considerations, such as safety and cost, ensured that its impact reached beyond academic theory to real-world application. As a next step, stakeholders in healthcare should prioritize integrating this strategy into clinical guidelines while supporting further studies to refine its implementation. Expanding access through policy changes and funding for advanced imaging could turn this innovation into a standard of care, ensuring that women with dense breasts no longer face heightened risks due to diagnostic limitations. This milestone laid a foundation for a future where early detection became more equitable and effective for all.