Listen to the Article
Telehealth is at the center of modern care services, with over 50% of clinicians believing it helps them deliver more effective treatment and follow-ups. Historically, access to timely and quality healthcare has been a challenge, especially for people in rural areas, those with mobility issues, or patients managing chronic conditions. By connecting patients and providers remotely, telehealth makes care more accessible, efficient, and patient-centered while helping health practices grow more sustainably. Here’s a closer look at how telehealth is improving the medical industry.
Breaking Down Barriers to Access
Limited transportation options, long travel times, and a shortage of local healthcare facilities often prevent patients from getting the care they need. Telehealth removes these barriers by bringing providers directly to patients, anytime and from anywhere. Whether through video consultations, remote monitoring tools, or mobile health apps, virtual visits allow patients to connect with their doctors from the safety and convenience of their home.
This accessibility doesn’t just increase convenience; it improves continuity of care. Patients can engage with their doctors more frequently without the logistical hurdles that typically delay or discourage medical follow-through.
For healthcare providers, this care continuity brings measurable business value, including:
Broader reach into underserved areas without needing to open new physical sites.
Reduced no-show rates due to improved ease of access.
More consistent patient flow, resulting in steadier and more predictable revenue growth.
Integrating telehealth into practices opens new channels of care and allows organizations to grow strategically and meet diverse patient needs.
Driving Patient Engagement and Satisfaction
By streamlining care delivery, telehealth increases patient engagement, which is a key driver of better outcomes and preventive care. Higher engagement makes the healthcare experience more convenient and flexible, reducing friction in the care process. Patients can book appointments more easily, avoid long waits, and attend follow-ups during their lunch break or after work, making it much more likely they will stick to their care plans.
Engaged patients are more likely to:
Take medications as prescribed.
Monitor symptoms and communicate changes.
Participate in lifestyle changes and maintenance programs.
In chronic care management, consistent virtual visits help patients stay on track and avoid costly ER visits. They also help foster stronger provider-patient relationships, which build trust and loyalty, which are essential ingredients for long-term health success.
From the provider’s perspective, engaged patients are more likely to return, follow medical advice, and provide positive feedback and referrals. This leads to better outcomes, higher patient satisfaction scores, and greater reimbursement potential under value-based care models.
Managing Chronic Conditions with Ease
Chronic diseases like diabetes, heart disease, and hypertension account for roughly 90% of the U.S. healthcare spend, making effective long-term management critical both for patient welfare and cost containment.
Telehealth plays a crucial role in addressing this need by enabling continuous, real-time care. With remote monitoring tools and connected wearables, patients can track key health indicators, such as blood sugar, blood pressure, or heart rate, and share that data instantly with their providers.
This approach shifts chronic disease management from reactive to proactive, improving health outcomes. Instead of waiting for symptoms to get worse, providers can intervene quickly, adjusting medications or offering lifestyle guidance before issues escalate.
Actively treating patients leads to:
Fewer ER visits and hospitalizations.
Better disease control and prevention.
Enhanced patient confidence and empowerment.
For healthcare organizations, better chronic care management reduces high-cost, high-risk episodes while improving patient retention and satisfaction over time.
Cutting Healthcare Costs
Telehealth doesn’t just benefit patients and providers clinically. It also drives significant cost savings.
For patients, the savings include:
Minimal transportation or parking fees.
Fewer missed workdays or childcare complications.
Lower up-front costs for certain types of virtual care visits.
For providers, telehealth means:
Reduced need for physical space, utilities, and on-site staff.
Streamlined scheduling, check-in, and documentation through digital platforms.
Less investment in patient throughput infrastructure, such as large waiting rooms.
Practices can reallocate resources to higher-value activities, such as chronic care programs or patient education efforts. These financial efficiencies make it easier for smaller or independent practices to remain viable while meeting growing demand for convenience and flexibility.
Timely Interventions Improve Health Outcomes
In healthcare, speed and precision save lives. Delayed diagnoses often lead to worsened conditions, complications, and costly interventions. Telehealth provides patients with faster access to care when symptoms first appear, without waiting days or even weeks for an appointment. This immediacy allows providers to identify and treat health concerns before they become chronic.
Examples of timely interventions via telehealth include:
Real-time adjustments to medications based on remote monitoring data.
Early evaluation of potential infections, avoiding hospitalizations.
Ongoing therapy for mental health conditions to prevent relapse or crisis episodes.
Adopting this fast-track approach improves clinical outcomes and reduces the unnecessary use of high-cost facilities like emergency rooms or inpatient wards. It allows clinicians to maintain high standards of care while optimizing operational expenses.
Improving Provider Efficiency
Telehealth also streamlines clinical workflows by helping providers make better use of their time and resources. Administrative load is significantly lessened through automation: think digital consent forms, remote intake, virtual check-ins, and EMR integration. As a result, providers spend less time on non-clinical tasks and more time delivering quality care.
The key operational benefits of simpler workflows include:
More flexible scheduling.
Fewer appointment gaps.
Higher provider availability, including after-hours care.
Cross-location coverage.
Collaboration, where providers can see more patients in less time.
Practices that adopt telehealth often report higher staff satisfaction, improved care coordination, and lower burnout among physicians and clinical teams.
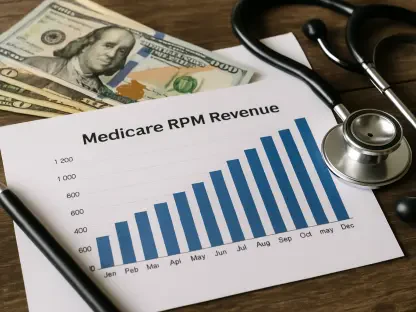
Delivering a Stronger ROI for Healthcare Practices
When implemented effectively, telehealth becomes a strategic growth engine. It increases top-line revenue, reduces bottom-line costs, and supports scalable care delivery models.
Telehealth unlocks new revenue by:
Allowing providers to expand their patient panels.
Enabling new billable services such as remote patient monitoring and chronic care management.
Reducing cancellations and improving appointment adherence.
Blending virtual with in-person care models gives providers the flexibility to design services that align with patient preferences and operational goals. This drives better utilization of resources and builds a more resilient, future-ready practice.
Telemedicine practitioners admit job effectiveness and productivity are direct advantages of integrating technology, with 59% crediting it for supporting higher performance that increases revenue. In the long run, telehealth enables practices to grow bigger and smarter, with a more sustainable balance of care quality, provider wellbeing, and business performance.
The Future: More Innovation, More Impact
Telehealth’s potential is far from being fully realized. The rapid pace of technological advancements promises even greater benefits in the near future. AI, machine learning, and data analytics are already being integrated into telehealth platforms to deliver more personalized, proactive care.
For example, predictive analytics may allow providers to anticipate potential health risks before they become serious, enabling even earlier intervention. Additionally, electronic health records seamlessly integrate into medical infrastructure to enhance the continuity of care with updated information. As time goes on, telehealth will become increasingly capable of managing complex care as these developments improve.
At the same time, its role in healthcare will continue to grow, providing more efficient, targeted, and patient-centered services. As technology advances, telehealth will become even more reliable and effective at preventing health issues and delivering personalized care. This translates into better experiences and outcomes for patients, and more innovative, cost-effective solutions for healthcare providers.
Conclusion
Telehealth is transforming healthcare delivery, bridging access gaps, enhancing patient engagement, and enabling better care at lower cost. For patients, it means timely support and greater control over their health. For providers, it offers new opportunities for growth, efficiency, and impact.
As adoption continues to rise and digital health tools become more sophisticated, telehealth will only grow in its capacity to improve outcomes and drive ROI. Now is the time for healthcare organizations to invest in building a telehealth strategy that is patient-focused, financially sound, and ready for the future.