The U.S. healthcare system is teetering on the edge of collapse, burdened by astronomical costs and systemic shortcomings that undermine its ability to serve the population effectively. Recent data reveals that healthcare spending soared to $4.9 trillion in 2023, representing 17.6% of the nation’s GDP, with projections indicating an even steeper climb over the next decade, potentially nearing 20% of GDP. This financial strain, paired with worsening health outcomes and glaring inequities in access, signals a profound failure to deliver value for the immense resources poured into the system. Patients face escalating out-of-pocket expenses, providers grapple with burnout, and payers struggle to manage spiraling costs. This article delves into the critical challenges plaguing healthcare in the United States, examining the root causes of unaffordability, declining health metrics, delivery imbalances, and the mixed outcomes of innovative solutions, while highlighting the pressing need for transformative change to avert further deterioration.
Financial Strain and the Affordability Barrier
The relentless rise in healthcare costs has become an unbearable weight on the U.S. economy and its citizens, creating barriers that many cannot overcome. Between 2009 and 2023, healthcare prices surged by 54.5%, far outstripping the general inflation rate of 45.7% over the same period. This disparity has driven average annual premiums for commercial insurance plans up by a staggering 85.7% since 2010, placing an immense burden on individuals, employers, and insurers alike. The consequence is a vicious cycle often termed a “doom loop,” where escalating costs deter patients from seeking timely care, leading to worse health outcomes that, in turn, drive expenses even higher. This financial pressure not only limits access but also erodes trust in a system that seems to prioritize profit over well-being, leaving millions struggling to afford even basic medical services while stakeholders scramble for solutions that remain frustratingly out of reach.
Another dimension of this affordability crisis lies in the broader economic impact and the strain it places on systemic sustainability. Representing nearly a fifth of GDP, healthcare spending diverts resources from other critical areas like education and infrastructure, hampering national growth. For employers, rising premiums translate into higher operational costs, often forcing tough choices between offering benefits and maintaining profitability. Meanwhile, patients increasingly face high-deductible plans that shift more financial responsibility onto their shoulders, discouraging preventive care and exacerbating long-term health issues. This creates a ripple effect, where delayed treatments lead to more complex, costly interventions down the line. The data paints a stark picture of a system where financial barriers are not just a symptom but a driving force behind declining access and worsening outcomes, underscoring the urgent need to rethink how costs are managed and distributed across the healthcare landscape.
Health Outcomes and Demographic Challenges
Health outcomes in the United States paint a troubling contrast to other developed nations, revealing a population grappling with preventable decline. Despite massive spending, life expectancy remains stagnant, with the average American enduring 12.5 years in poor health—a far cry from OECD counterparts who often live four to eight years longer in better condition. Avoidable mortality rates are alarmingly high, and chronic disease deaths among younger adults aged 18-44 have risen by 6.4% in recent years, driven by conditions such as chronic liver disease. These metrics highlight a failure to prioritize early intervention and lifestyle management, leaving the population vulnerable to conditions that could often be mitigated with proper care. The disparity in health outcomes raises critical questions about why such a resource-rich system struggles to deliver results that match its investment, pointing to deeper structural flaws.
Compounding these health challenges are demographic shifts that the healthcare infrastructure is ill-prepared to address. Significant population movements toward Sunbelt states, coupled with declines in traditional hubs like California and New York, are reshaping where care is needed most. Yet, the system has been slow to adapt, resulting in overburdened facilities in growing regions and underutilized resources elsewhere. This mismatch exacerbates access issues, particularly for aging populations and those with chronic conditions who require consistent care. Additionally, the increasing prevalence of lifestyle-related illnesses reflects broader societal trends that healthcare alone cannot solve, necessitating collaboration with public health initiatives. These geographic and demographic dynamics underscore the need for a more agile, responsive framework that can anticipate and meet evolving demands rather than react to crises after they emerge.
Delivery Imbalances and Systemic Inefficiencies
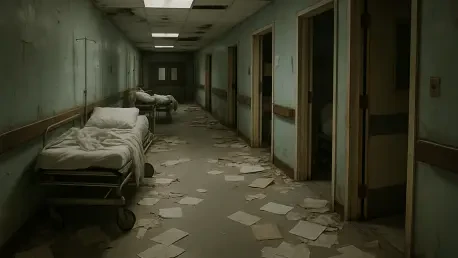
The structure of healthcare delivery in the U.S. reveals a troubling bias toward expensive specialty care at the expense of foundational primary care, perpetuating inefficiencies. With chronic conditions like long COVID and behavioral health issues on the rise, the system’s focus on reactive, high-cost interventions over prevention leaves many needs unmet. A persistent shortage of primary care physicians further tilts the balance, forcing patients into emergency settings for issues that could have been managed earlier. Moreover, pervasive issues like fraud, waste, and abuse inflate costs through inconsistent pricing models and excessive administrative overhead. Even tools meant to streamline operations, such as electronic health records, often fail to deliver promised efficiencies, instead adding complexity without enhancing patient or provider experiences. This skewed approach highlights a fundamental misalignment in priorities that undermines the system’s ability to serve its core purpose.
Further deepening these systemic flaws is the inability of major disruptors to effect lasting change within the healthcare space. The retreat of prominent retail giants from healthcare ventures illustrates the formidable barriers to innovation in an industry riddled with entrenched interests and regulatory hurdles. Hospitals, often burdened by disproportionate administrative spending, contribute to cost inflation without corresponding improvements in care quality. Meanwhile, intermediaries like brokers and pharmacy benefit managers add layers of expense and opacity, further distancing patients from affordable solutions. These inefficiencies are not merely financial but also erode trust, as patients and providers alike navigate a labyrinthine system that often prioritizes bureaucracy over health outcomes. Addressing these delivery imbalances requires a hard look at simplifying processes and refocusing on connecting patients with essential care rather than perpetuating a cycle of complexity and waste.
Innovation’s Promise and Persistent Gaps
Efforts to modernize healthcare through alternative care models and technology have shown both potential and limitations, reflecting a system in uneasy transition. Telehealth, which surged during the pandemic, has since declined by 32.2% from its 2020 peak, though it remains vital for behavioral health, accounting for 66.9% of visits. Outpatient settings like ambulatory surgical centers are increasingly utilized for procedures once confined to hospitals, signaling a shift toward more cost-effective care delivery. Additionally, the use of GLP-1 drugs for weight management has skyrocketed by 744.6% since 2018, often facilitated through virtual platforms. However, these advancements are unevenly distributed, with rural areas facing shrinking inpatient services that worsen access disparities. Such trends reveal that while innovation can address specific pain points, it often falls short of tackling the broader structural challenges that continue to hinder equitable care.
Another layer of complexity in this innovation landscape is the struggle to sustain momentum and scale solutions effectively across diverse populations. The post-pandemic drop in telehealth usage, particularly for non-behavioral care, suggests that technological adoption faces barriers like digital literacy and infrastructure gaps, especially in underserved communities. Meanwhile, rural healthcare’s decline highlights a geographic divide that no amount of virtual care can fully bridge without targeted investment in physical resources. Even promising pharmaceutical advances, while impactful for some, raise questions about long-term affordability and accessibility as costs remain prohibitive for many. These mixed outcomes underscore that innovation alone cannot overhaul a system steeped in inefficiency; it must be paired with policy reforms and strategic resource allocation to close persistent gaps and ensure that advancements benefit all segments of society rather than a privileged few.
Path Forward Amidst Deep-Rooted Challenges
Reflecting on the state of U.S. healthcare, it has become evident over recent years that the system has reached a critical juncture, with costs spiraling out of control and outcomes failing to justify the investment. The data from 2023, showing expenditure at $4.9 trillion, has already sounded alarms that echo through every stakeholder group, from patients to policymakers. Systemic imbalances, coupled with demographic pressures, have exposed vulnerabilities that no quick fix can mend. Even innovations, once heralded as game-changers, have shown their limits by failing to address core access and affordability issues. The struggles of that period paint a clear picture of a framework trapped in its own complexity, unable to prioritize the fundamental connection between patients and essential care without drastic intervention.
Looking ahead, the focus must shift to actionable strategies that dismantle entrenched inefficiencies and rebuild trust in healthcare delivery. Streamlining administrative processes and curbing fraud could redirect billions toward patient care, while incentivizing primary care investment might rebalance the system away from costly specialty interventions. Policymakers should explore bolder reforms, such as pricing transparency and middleman elimination, to reduce financial barriers. Simultaneously, targeted support for rural infrastructure and telehealth expansion could address geographic disparities, ensuring no community is left behind. Collaboration between government, industry, and public health entities will be crucial to align incentives around value rather than volume. Only through such comprehensive, forward-thinking measures can the healthcare system move beyond past failures and forge a sustainable path that prioritizes health over profit.