From Crisis Response to Clinical Mainstay: Redefining the Role of Virtual Visits
The landscape of primary care, once fundamentally reshaped by the urgent demands of the COVID-19 pandemic, has settled into a new and durable equilibrium. The era of dramatic telehealth fluctuations—marked by an explosive surge and a subsequent recalibration—has given way to a period of remarkable stability. Comprehensive research reveals that since 2023, virtual appointments have consistently accounted for approximately 6% to 7% of all primary care visits. This stabilization signals more than just a trend; it marks the establishment of a new baseline where telehealth is no longer an emergency stopgap but an integrated and permanent fixture in healthcare delivery. This article explores the journey to this new normal, dissecting the demographic, geographic, and policy factors that define the current state of virtual primary care and shape its future trajectory.
The Pandemic’s Catalyst: Tracing the Rise and Recalibration of Virtual Care
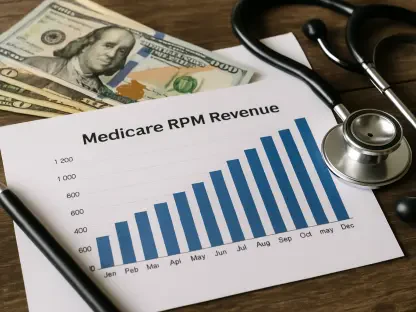
The integration of telehealth into mainstream primary care was massively accelerated by the global health crisis. Before 2020, virtual visits were a niche offering, but the pandemic transformed them into a critical tool for ensuring continuity of care while minimizing viral transmission. This rapid adoption was enabled by pivotal federal policy changes that expanded Medicare reimbursement for a wide array of telehealth services and relaxed regulations on the virtual prescription of certain medications. However, as the public health emergency waned, a natural market correction occurred. Data shows a significant decline from the pandemic-era peaks; for instance, after accounting for over 8% of primary care encounters in July 2022, telehealth usage dropped by nearly 30% to just under 6% by late 2025. The crucial insight is not the decline itself, but the plateau that followed. This sustained level of use demonstrates that telehealth has successfully carved out a meaningful, permanent role, contrasting sharply with specialties like mental healthcare, where it remains the dominant modality for over a quarter of all visits.
Dissecting the DatKey Factors Shaping Telehealth Utilization
The Digital Divide: Unpacking Geographic and Infrastructural Disparities
While the national average points to a stable integration of telehealth, a closer look at the data reveals profound disparities in its adoption. Geography emerges as a primary determinant, with patients in metropolitan areas utilizing virtual care at approximately double the rate of those in rural communities. This finding highlights a critical paradox: while telehealth holds immense promise for bridging access gaps for rural populations facing provider shortages and long travel times, its potential remains unrealized. Systemic barriers, including the financial strain on smaller rural hospitals to implement robust telehealth systems and the persistent lack of reliable high-speed internet access in many non-urban regions, continue to hinder equitable adoption and perpetuate the very access issues telehealth was meant to solve.
A Generational Snapshot: How Age Shapes Telehealth Adoption Rates
Age is another key factor influencing the preference for virtual versus in-person care. The highest rates of telehealth utilization are found among working-age adults, particularly those between 25 and 39, who used virtual services for roughly 10% of their primary care needs. This cohort often values the convenience and flexibility that telehealth affords. Conversely, adoption rates were lowest at the opposite ends of the age spectrum. Pediatric patients aged 0-2 and the oldest geriatric cohorts both showed utilization rates below 2%. This pattern suggests that for the youngest and oldest patients, the necessity of physical examinations, hands-on diagnostics, and direct provider-patient interaction makes traditional in-person care the overwhelmingly preferred and often clinically necessary modality.
Beyond the Obvious: The Surprising Influence of Language and Policy
In a finding that challenges previous assumptions, the research indicates that patients with limited English proficiency are among the most active users of telehealth. Individuals who primarily speak Chinese, Portuguese, Russian, Persian, or Spanish demonstrated consistently higher rates of virtual care adoption than native English speakers. While the precise reasons require further study, experts speculate that factors like the increased availability of virtual translation services, the convenience of avoiding complex transportation, and the ability to fit appointments around work schedules may contribute to this trend. This dynamic is further supported by a stabilizing policy environment. The recent extension of key Medicare telehealth flexibilities through the end of 2027 provides the regulatory certainty needed for healthcare systems to confidently invest in and refine their virtual care offerings, cementing telehealth’s role in the national healthcare ecosystem.
Charting the Course Forward: Policy Stability and the Future of Hybrid Care
With a new baseline established and regulatory uncertainties largely settled for the near future, the focus is shifting from adoption to optimization. The extension of Medicare coverage provides a crucial runway for healthcare organizations to move beyond reactive telehealth implementation and toward a more intentional, integrated hybrid care model. The future will likely see greater investment in technologies that seamlessly blend virtual and in-person touchpoints, creating a more cohesive patient journey. This stability also allows providers and policymakers to address the disparities uncovered in the data, potentially driving targeted initiatives to improve digital literacy and expand broadband infrastructure in underserved rural areas. The next phase of telehealth evolution will not be about growth, but about refinement, equity, and strategic integration.
Strategic Imperatives for a Hybrid Healthcare Future
The stabilization of telehealth in primary care yields several major takeaways for stakeholders across the healthcare industry. First, the 6-7% utilization rate represents a permanent shift, and providers must treat virtual care as a core service line, not an optional add-on. Second, the significant disparities in adoption based on geography and age highlight the need for tailored strategies; a one-size-fits-all approach to telehealth will fail. For healthcare leaders, the key recommendation is to develop a deliberate hybrid care strategy that defines which services are best suited for virtual delivery and which require in-person visits, ensuring clinical appropriateness and equitable access. For policymakers, the focus must be on closing the digital divide by investing in the infrastructure and training needed to make telehealth a viable option for all Americans.
Embracing the New Balance in Patient Care
The journey of telehealth in primary care—from a fringe service to a crisis necessity and now to a stable component of routine healthcare—is a story of profound and rapid evolution. It has found its new normal, a balanced integration that leverages technology to enhance convenience and access while preserving the irreplaceable value of in-person medicine. The challenge ahead is not to increase its use for the sake of it, but to refine its application, ensuring it effectively serves the diverse needs of all patient populations. By embracing this new equilibrium, the healthcare industry can build a more resilient, efficient, and patient-centered system for the future.