A staggering 80 to 90 percent of an individual’s health outcomes are shaped not by doctor visits or prescriptions, but by lifestyle and environmental factors that remain invisible to traditional medical records. This fundamental disconnect lies at the heart of a persistent interoperability crisis within the American healthcare system, where the integration of data on Social Drivers of Health (SDoH) has been largely unsuccessful. Clinicians are often left with poor, unusable data, contributing to dissatisfaction and hindering their ability to provide comprehensive care. In a landmark move to address this challenge, Healthconnect Texas and the Patient Care Intervention Center (PCIC) have strategically unified their operations. This merger is designed to create a comprehensive infrastructure that directly confronts the data gap, aiming to provide a true “360-degree view” of patient wellness by weaving together statewide clinical connectivity with deep, community-based insights on the non-medical factors that define a person’s health journey.
Bridging the Gap Between Clinic and Community
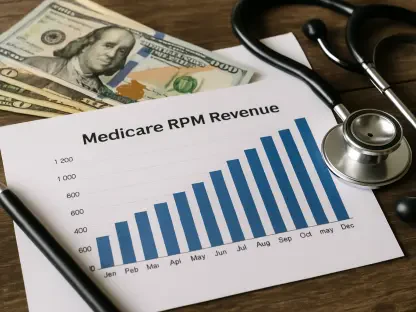
The newly formed entity’s strategy hinges on the powerful synthesis of disparate data sources, merging real-time clinical information with vital community-level intelligence on housing, nutrition, and transportation. This integration is not merely about data collection; it is about creating an automated, seamless exchange of records between clinical settings and community-based organizations. By doing so, the initiative facilitates a new standard of coordinated, whole-person care where a physician can understand a patient’s food insecurity with the same clarity as their lab results. This “plug-and-play” solution offers Texas health systems a streamlined pathway to meet increasing mandates from the Centers for Medicare & Medicaid Services (CMS) for enhanced data sharing and a greater focus on health equity. Beyond individual patient care, this aggregated, contextualized data serves as a powerful engine for change, fueling actionable insights for researchers and policymakers dedicated to identifying and reducing systemic health disparities for a population of 30 million.
The Cornerstone of Interoperability
Ultimately, the initiative revealed that the greatest challenge to achieving a holistic view of health was not a matter of technology, but of trust. Industry analysis has consistently shown that building robust patient privacy protocols and fostering genuine trust among patients, providers, and community partners are more critical to successful data sharing than any software or platform. The joint organization began its unified operations immediately, with the launch of new integrated services in early 2026 marking a key milestone in its development. This approach reframed the entire concept of interoperability, moving it from a technical requirement to a strategic asset built on a foundation of confidence and collaboration. By successfully closing the gap between sterile clinical data and the rich context of a person’s daily life, the project demonstrated how a trust-centric model could transform data exchange into a powerful tool for improving long-term health outcomes on a massive scale.