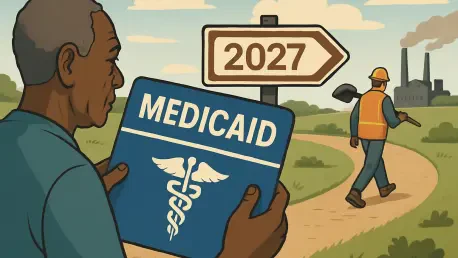
Imagine a policy shift so monumental that it could reshape healthcare access for millions of low-income Americans while saving billions in federal spending, a reality states face with the mandate to implement work requirements for Medicaid beneficiaries by 2027. Enacted through a landmark tax and policy law under Republican leadership, this overhaul—the most significant in Medicaid’s 60-year history—requires adults aged 19 to 64 under the Affordable Care Act (ACA) expansion to complete 80 hours per month of work, education, or community service to retain coverage. With fewer than two years remaining, states are in a race against time to adapt systems, manage budgets, and address ethical dilemmas. This market analysis explores the trends, data, and projections surrounding this transformative policy, shedding light on operational hurdles, financial implications, and strategic pathways forward in the healthcare policy landscape.
Diving Deep: Trends, Data, and Projections in Medicaid Policy Implementation
Unpacking the Policy Drivers and Market Pressures
The push for Medicaid work requirements stems from a federal goal to curb spending, with projections from the Congressional Budget Office (CBO) estimating savings of $330 billion over a decade. This policy targets a significant portion of the healthcare market, affecting millions enrolled under ACA expansion in 40 states and Washington, D.C. However, the urgency of the 2027 deadline creates intense pressure on state governments, which must balance compliance with the risk of coverage losses. Data from past pilot programs in states like Arkansas reveals a sobering trend: minimal employment gains coupled with substantial disenrollment due to administrative barriers. This historical pattern signals a market risk—potentially shrinking the insured population and impacting healthcare providers reliant on Medicaid reimbursements.
Operational Challenges Shaping State Readiness
State healthcare systems are grappling with operational bottlenecks as they overhaul data tracking and eligibility frameworks. A Georgetown McCourt School of Public Policy analysis indicates that over half of the states lack the infrastructure to meet the looming deadline. Georgia, currently the only state with an active program, has encountered technical failures such as portal crashes, leading to improper coverage terminations. These issues highlight a broader market concern: inadequate IT systems could disrupt service delivery and strain provider networks. With federal funding limited to $200 million in 2026—roughly $4 million per state—states face a resource crunch that could exacerbate disparities in implementation capacity across regions.
Financial Dynamics and Budgetary Strain on States
Medicaid already accounts for approximately 30% of state budgets, and the added burden of implementing work requirements intensifies fiscal challenges. The minimal federal allocation falls short of covering costs for system upgrades and outreach efforts, creating a market dynamic where states must reallocate existing funds or risk noncompliance. Projections suggest that delayed federal support or unclear funding distribution timelines could derail progress, particularly for states with constrained 2026 budgets. This financial tension underscores a critical market implication: states may prioritize cost-cutting over comprehensive implementation, potentially reducing access to care and affecting healthcare delivery sectors.
Ethical and Coverage Implications in the Healthcare Market
Beyond logistics, the policy stirs ethical debates within the healthcare market about its true intent. Critics view work requirements as a mechanism to slash federal expenditure by reducing enrollment, rather than fostering self-reliance. Historical data supports this concern, showing that past mandates led to significant coverage losses without notable employment increases. The CBO forecasts that millions could lose coverage by 2027, often due to documentation hurdles rather than noncompliance. This trend poses a risk to market stability, as reduced enrollment could lower demand for Medicaid-funded services, impacting hospitals and clinics serving low-income populations.
Emerging Trends and Technological Opportunities
Looking toward the next two years, technological innovation stands out as a pivotal trend in navigating this policy shift. Modernized IT systems could streamline compliance tracking and minimize errors, offering a market opportunity for tech vendors specializing in healthcare solutions. However, funding constraints may slow adoption, particularly in less-prepared states. Another trend is the potential for community partnerships to bridge communication gaps, with local organizations like health centers playing a role in educating beneficiaries. Additionally, regulatory uncertainties—such as ambiguous Centers for Medicare & Medicaid Services (CMS) guidance on exemptions—could shape market responses, as states may face legal challenges or policy adjustments before 2027.
Reflecting on the Analysis: Key Takeaways and Strategic Pathways
Looking back, this analysis revealed the multifaceted challenges states encounter in implementing Medicaid work requirements under a tight 2027 deadline. The policy’s focus on federal savings clashes with operational realities, as outdated systems and limited funding hinder progress. Coverage losses loom large, driven by historical patterns of administrative barriers rather than genuine noncompliance, while state disparities underscore uneven market impacts. Moving forward, states should prioritize investments in IT infrastructure to ensure accurate tracking and prevent disruptions. Strengthening community outreach through trusted local entities could mitigate beneficiary confusion and coverage gaps. Additionally, advocating for clearer CMS guidance on exemptions and funding timelines would provide a foundation for equitable implementation. As the healthcare market braces for this transformation, strategic collaboration between states, federal agencies, and private sector players will be essential to balance fiscal goals with the imperative to protect vulnerable populations.