Managing denials and appeals is a critical aspect of Revenue Cycle Management (RCM) that significantly impacts the financial health of healthcare providers. Despite its importance, many providers struggle with the complexities involved. In an environment where financial sustainability and operational efficiency are paramount, mastering the intricacies of denials and appeals becomes indispensable. Understanding the causes of denials, implementing preventative measures, leveraging technology, and maintaining a structured appeals process are integral to achieving optimal RCM performance. This article explores practical strategies for effectively managing denials and appeals to ensure the financial stability and smooth operation of healthcare institutions.
Understanding Denials in Healthcare RCM
Denials in healthcare RCM occur when payers, such as insurance companies, refuse to reimburse for the services provided by healthcare institutions. Common causes for these denials include coding errors, administrative oversights, and failures to verify insurance coverage thoroughly. Each of these causes necessitates a comprehensive review and correction process, which is often both time-consuming and costly. Coding errors, for instance, might stem from mismatches between services rendered and billing codes used, while administrative oversights may include incomplete patient information and lack of prior authorizations. The complexities surrounding denials make them a significant challenge for healthcare providers to manage effectively.
Denials also impact operational efficiency by delaying payments and requiring extensive administrative follow-up to rectify the issues. The resources allocated to managing denials put a strain on operational capacities, often resulting in financial stress for healthcare providers. Hospitals and clinics must dedicate expensive manpower and time to resolve each denial, diverting resources from other critical functions. Understanding these complexities is the foundational step toward overcoming challenges associated with denials. It also underscores the necessity for healthcare institutions to adopt robust and systematic approaches to manage and mitigate the occurrence of denials effectively.
Impact of Denials on Financial Health
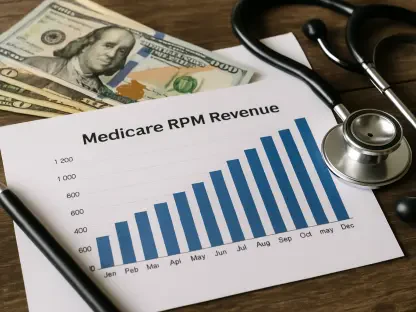
The financial implications of denials are substantial, and addressing them is essential not only for maintaining cash flow but also for improving overall financial health. With rework costs per denial ranging anywhere from $25 to $181, even institutions with a small denial rate can experience significant financial strain. For healthcare providers with average denial rates reaching up to 20%, reducing denials can translate into considerable cost savings. These financial pressures highlight the urgent need for effective denial management strategies. Reducing the incidence of denials not only helps conserve financial resources but also allows for the reallocation of funds toward enhancing the quality of patient care and ensuring the institution’s long-term sustainability.
Timely payments facilitated by reducing denials ensure that healthcare providers can continue to invest in quality care and resources for their patients. When denials are minimized, cash flows remain steady, contributing to the financial performance and operational viability of the healthcare institution. Consequently, effective management of denials is crucial for sustained financial performance. It enables healthcare providers to avoid the pitfalls associated with delayed reimbursements and high administrative costs, ultimately leading to a more robust RCM process. By focusing on reducing denials, healthcare institutions can improve their financial health and maintain a continuous cycle of service and care for their patients.
Preventative Measures: Front-End Processing
Preventative measures play a pivotal role in reducing denials, with robust front-end processing being instrumental in this endeavor. Front-end processing encompasses meticulous patient data collection, thorough insurance verification, and strict adherence to coding protocols. By ensuring accuracy at this preliminary stage, healthcare institutions can prevent many of the common errors that lead to denials. Meticulous patient data collection involves verifying the completeness and correctness of all patient information before the services are rendered. Thorough insurance verification helps in confirming the patient’s coverage and obtaining necessary pre-approvals, reducing the chances of claims being denied due to lack of authorization or coverage issues.
Regular staff training and periodic audits significantly enhance the accuracy of front-end processes. Training sessions keep the staff updated on the latest coding standards, payer requirements, and best practices, thereby reducing the likelihood of errors. Periodic audits are essential in identifying and rectifying recurring errors within the system, allowing for continuous improvement. By implementing these preventative measures, healthcare institutions can proactively minimize denials, ensuring a smoother RCM process. The combined effect of accurate data collection, stringent insurance verification, and ongoing staff education and audits culminates in a more efficient and error-free front-end process.
Leveraging Technology to Reduce Denials
Modern Revenue Cycle Management solutions can significantly reduce denials by integrating advanced technology into the claims process. Sophisticated claim scrubbing software represents one such technological intervention, preemptively identifying potential errors to ensure claim accuracy before submission. By catching discrepancies early, it prevents denials from occurring, thereby streamlining the reimbursement process. Technology also facilitates seamless communication among various departments, ensuring that any potential issues are addressed promptly. This technological intervention is essential for healthcare providers aiming to maintain an efficient RCM process since it helps reduce administrative burden and improves the flow of operations.
Additionally, data analytics tools further aid in denial management by identifying trends and patterns associated with past denials. By analyzing historical data, healthcare providers can pinpoint common pitfalls in their billing processes and implement targeted improvements. These analytics tools can highlight specific areas where errors frequently occur, allowing institutions to focus their efforts on the most impactful changes. Leveraging technology in this manner ensures that healthcare providers can continuously refine their RCM processes, staying ahead of potential issues and maintaining a high level of efficiency. The integration of technological solutions is a crucial strategy for any healthcare institution looking to mitigate the impact of denials and enhance their overall operational effectiveness.
The Appeals Process: Structured and Timely
When denials do occur, an effective appeals management process becomes vital. The process begins with a thorough review of denial notices to understand the exact reasons for rejection. This initial review is critical, as it informs the subsequent steps in the appeals process. Gathering necessary documentation and constructing a robust appeal are essential for a successful outcome. This includes compiling medical records, authorization forms, and any other pertinent information that can substantiate the claim. A well-documented appeal is more likely to result in a successful overturn of the denial, facilitating timely reimbursement.
Timely filing is another critical component of the appeals process. Payers often have specific deadlines for filing appeals, and missing these deadlines can permanently obstruct the recovery of due funds. Adhering to these timelines ensures that appeals are reviewed and processed in a timely manner. Persistent follow-up is equally important, involving regular communication with payers and swift provision of additional information when needed. Keeping track of the appeal status, responding promptly to payer inquiries, and maintaining an open line of communication are vital for keeping the appeal in progress. This structured and timely approach to the appeals process is essential for recovering denied funds and ensuring a steady cash flow for healthcare institutions.
Challenges in Government-Dominated Payor Environments
Healthcare institutions heavily reliant on government payors like Medicare and Medicaid face unique challenges that add layers of complexity to the RCM process. With approximately 85% of revenue coming from these government programs, strict reimbursement criteria and complex billing protocols become significant hurdles. Medicare and Medicaid often have more stringent documentation and coding requirements, making it easier for claims to be denied if not meticulously managed. This high level of scrutiny demands that healthcare providers maintain exceptional precision in their billing and coding practices. Any oversight can result in denials that require exhaustive efforts to appeal and rectify.
Operating under tight financial constraints, many of these institutions frequently run at negative margins, making every claim vital for financial survival. Accurate and efficient denial and appeal management ensures that necessary resources are available for essential healthcare services, emphasizing the importance of meticulous RCM practices. Institutions serving a large proportion of government-insured patients must invest in robust systems and staff training to navigate the complexities of government reimbursement protocols effectively. The pressure to adhere to these complex requirements while maintaining financial viability underscores the critical role of precise and efficient RCM in these environments.
Increasing Complexity and Proactive Measures
Managing denials and appeals is a vital component of Revenue Cycle Management (RCM) that greatly impacts the financial health of healthcare providers. Despite its significance, many providers find it challenging to navigate the complexities involved. In a setting where financial stability and operational efficiency are crucial, mastering the nuances of denials and appeals becomes essential. Understanding the reasons behind denials, implementing preventive strategies, leveraging advanced technology, and maintaining a structured appeals process are key elements to achieving optimal RCM performance. Without these elements, healthcare institutions risk financial instability and operational disruptions. This article explores practical tactics for effectively managing denials and appeals, highlighting the importance of these strategies in ensuring the financial stability and efficient operation of healthcare organizations. By focusing on these aspects, healthcare providers can better manage their revenue cycles, reduce losses, and sustain their financial health, ultimately leading to improved patient care and service quality.