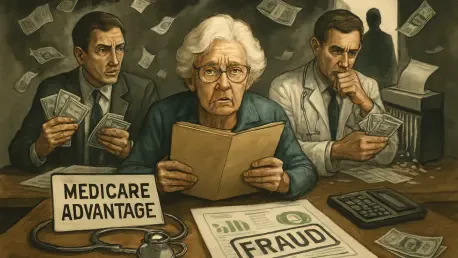
What happens when a program designed to save money for seniors and taxpayers turns into a goldmine for corporate giants? Medicare Advantage, a privatized healthcare option meant to streamline costs for millions of older Americans, is at the center of a staggering controversy. Reports reveal that major insurers are exploiting loopholes to rake in billions annually, leaving taxpayers footing the bill. This eye-opening situation demands a closer look at how a system built on trust is being manipulated for profit, and what can be done to reclaim fairness.
The Broken Promise of Cost Savings
Medicare Advantage (MA) was introduced as a beacon of efficiency, a private alternative to traditional Medicare that promised better care at lower costs. With over half of Medicare enrollees now under MA plans, the program has grown into a massive industry. However, beneath the surface lies a troubling reality: costs are spiraling out of control, not because of sicker patients, but due to systemic exploitation by some of the largest players in the field.
The significance of this issue cannot be overstated. Taxpayer dollars, intended to support healthcare for vulnerable seniors, are instead padding the bottom lines of corporate insurers. Independent analyses project that overpayments to MA plans could reach $600 billion over the next decade if unchecked. This financial drain threatens the sustainability of Medicare itself, raising urgent questions about accountability and reform.
Why Are Medicare Costs Exploding Under Private Plans?
A key driver behind the skyrocketing costs of MA lies in the structure of the program. The government pays private insurers a fixed fee per enrollee, adjusted based on health status to ensure fair compensation for managing sicker individuals. Yet, this risk adjustment system, meant to balance the scales, has become a tool for inflating payments far beyond what’s justified.
Data paints a grim picture of the financial impact. Studies estimate that MA payments are set to increase by 10% compared to traditional Medicare in the current year, driven largely by manipulated health scores. With total MA spending projected to hit nearly $8 trillion from this year to 2033, the stakes for taxpayers are enormous, highlighting a pressing need to address these excesses.
The burden falls not just on federal budgets but also on public trust. When costs explode without corresponding improvements in care, confidence in privatized healthcare erodes. This growing disparity between intent and outcome sets the stage for deeper scrutiny into how these plans operate.
The Profit Game: Tactics Insurers Use to Inflate Payments
At the heart of this financial scandal are specific strategies employed by major insurers to exploit the risk adjustment system. Practices like “upcoding”—where diagnoses are aggressively documented, often without follow-up treatment—allow companies to inflate risk scores and secure higher reimbursements. For instance, some insurers send nurses to enrollees’ homes solely to record additional health conditions, prioritizing paperwork over patient care.
The numbers behind these tactics are staggering. One leading insurer reportedly gained over $6 billion in excess payments last year, while another added $4 billion through similar methods. These figures aren’t mere outliers; they reflect a calculated approach to maximize revenue, often at the expense of program integrity.
Beyond upcoding, other methods amplify the problem. Health assessments conducted without clinical necessity contribute to inflated scores, creating a cycle where profit trumps purpose. This systematic manipulation reveals a design flaw in MA that rewards documentation over genuine health outcomes.
Expert Alarms and Data-Driven Revelations
Voices from across the healthcare spectrum are sounding the alarm on these disparities. Michael Bagel, Vice President of Policy at the Alliance of Community Health Plans (ACHP), has pointed out that risk score differences of up to 36.2% between for-profit giants and nonprofit plans are highly unlikely to stem from real health variations. Instead, such gaps suggest deliberate gaming of the system.
Supporting these concerns, independent research offers hard evidence of the scale of abuse. Reports from groups like MedPAC and the Committee for a Responsible Federal Budget warn of massive overpayments, with long-term costs potentially crippling Medicare’s financial stability. These findings fuel a growing consensus that oversight is sorely lacking.
Bipartisan concern is also mounting on Capitol Hill, reflecting a rare unity on the need for action. As data continues to expose the depth of this issue, the pressure builds for policymakers to step in and prevent further erosion of public resources. The chorus of expert critique underscores that this is not a minor glitch but a systemic failure.
Steps Toward Reform and Accountability
Addressing this billion-dollar scandal requires concrete, actionable reforms to close the loopholes fueling overpayments. The ACHP has proposed a streamlined risk adjustment model, focusing on demographics like age and sex, alongside a limited set of verified health conditions. Such a shift could eliminate the incentives for upcoding by simplifying how payments are calculated.
Current efforts show some promise, with the Centers for Medicare & Medicaid Services (CMS) planning intensified audits to recover overpayments. Additionally, bipartisan legislation aims to exclude unsupported diagnoses from risk score calculations, a step that could save substantial funds. These initiatives, though still in progress, signal a willingness to tackle the problem head-on.
Public awareness and advocacy play a vital role as well. Staying informed about these issues and supporting policies that prioritize patient care over corporate gain can drive meaningful change. Redirecting even a fraction of misused funds toward actual healthcare needs could transform outcomes for millions of seniors.
Reflecting on a Path Forward
Looking back, the journey to expose and address the exploitation within Medicare Advantage revealed a stark betrayal of its founding principles. The billions siphoned through manipulated risk scores stood as a testament to unchecked corporate influence, straining public resources and trust. Each revelation, from expert critiques to damning data, painted a clearer picture of a system in crisis.
Yet, amidst the challenges, glimmers of hope emerged in the form of proposed reforms and growing political will. The push for a fairer risk adjustment model offered a blueprint for change, while CMS audits and legislative efforts hinted at accountability on the horizon. These steps, though incomplete, marked the beginning of a potential turnaround.
Moving ahead, sustained pressure on policymakers to prioritize transparency remains essential. Supporting initiatives that curb overpayments and redirect funds to patient care can reshape the landscape of privatized healthcare. The fight for a Medicare Advantage that truly serves seniors demands vigilance, ensuring that past abuses pave the way for a more equitable future.