Cancer care has seen a transformative impact with the advent of artificial intelligence, marking the evolution from basic rule-based systems to sophisticated deep learning platforms that significantly enhance oncologists’ decision-making. This evolution represents a pivotal moment in the integration of data-driven insights for clinical decisions. The synergy of artificial intelligence (AI) and machine learning (ML) in medical oncology introduces new dimensions of precision, personalization, and efficiency, fundamentally changing treatment strategies and enhancing patient outcomes.
Enhanced Treatment Strategies
AI algorithms possess the remarkable ability to analyze complex datasets, including tumor genomics and proteomics, which provides a deeper understanding of cancer mechanisms. These algorithms facilitate significant innovations in diagnosis, treatment planning, drug discovery, clinical decision support systems (CDSS), and data integration. In adult oncology, AI has notably improved imaging analysis and treatment planning. Moreover, AI’s contribution to enhanced drug discovery processes and more informed clinical decision support through CDSS has been profound, delivering precise radiomics for tumor characterization and assisting in radiation therapy planning to minimize damage to healthy tissues.
Innovations in Drug Discovery
The utilization of AI in drug discovery expedites the evaluation of extensive chemical libraries and predicts drug efficacy and toxicity, enabling the development of personalized treatment regimens. The profound impact of AI and its role in data integration allow for a comprehensive analysis of both clinical and molecular data. This streamlines treatment planning and patient monitoring, significantly bolstering clinical trial matching processes. Through the accelerated analysis of medical data, AI identifies suitable trial candidates based on diverse clinical characteristics, thereby enhancing the efficiency of patient recruitment.
Pediatric Oncology Challenges and Benefits
Pediatric oncology faces unique challenges, such as the rarity of certain malignancies and complex ethical considerations. Despite these obstacles, AI technology offers substantial benefits. AI aids in early and accurate diagnosis, risk stratification for hereditary cancers, and the development of personalized therapies tailored to the genetic and molecular profiles of pediatric patients. This significant shift towards AI-powered precision oncology promotes individualized treatment plans, aiming to maximize efficacy while minimizing adverse effects. The adoption of such approaches potentially reduces healthcare costs by avoiding ineffective treatments and optimizing resource utilization.
Emerging AI Trends
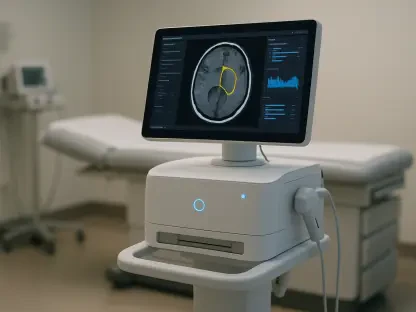
Emerging trends in AI, including computer vision, are revolutionizing procedures such as real-time biopsy guidance and precision-guided surgeries. These advancements not only enhance diagnostic accuracy but also improve surgical precision and overall patient outcomes. The integration of Explainable AI (XAI) technologies is particularly highlighted as crucial for maintaining trust and transparency in AI-driven decision-making processes. However, several ethical considerations and challenges, such as data privacy, algorithmic bias, and the need for clear regulatory frameworks, must be diligently addressed to ensure responsible use of AI in oncology.
Future Considerations
Looking ahead, the integration of AI with Electronic Health Records (EHRs) represents a significant advancement, allowing for real-time patient data analysis and the development of dynamic treatment strategies. The future also holds the promise of autonomous systems and the utilization of quantum computing, which are anticipated to further expand AI’s capabilities in cancer care. The vision is a future where AI and human expertise synergistically enhance cancer care, ensuring that technological advancements support, rather than replace, the physician-patient relationship.
Towards Optimal Care
The advent of artificial intelligence (AI) has revolutionized cancer care, transitioning from simplistic rule-based systems to advanced deep learning platforms that substantially improve oncologists’ decision-making processes. This technological progression marks a significant moment in the incorporation of data-driven insights into clinical decisions. The combination of AI and machine learning (ML) in medical oncology brings unprecedented levels of precision, personalization, and efficiency, fundamentally transforming treatment strategies and greatly enhancing patient outcomes. These technologies allow for more accurate diagnoses, tailored treatment plans, and predictive analytics, which optimally allocate resources and anticipate patient needs. In essence, the integration of AI and ML heralds a new era in oncology, where enhanced data interpretation plays a crucial role in improving the quality and effectiveness of cancer treatment, leading to better, more personalized patient care.