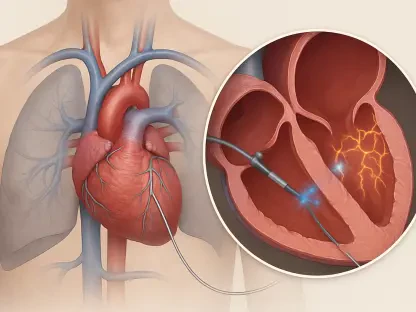
The unfortunate case of Caroline Kavanagh and her unborn son at Tipperary University Hospital highlights the severe repercussions of diagnostic errors within healthcare facilities. Ms. Kavanagh was admitted for chest pains at 22 weeks pregnant, a period that demanded meticulous evaluation. However, the evident oversight in distinguishing between pregnancy-related symptoms and potential cardiovascular issues led to a tragic outcome. Despite elevated Troponin levels, indicative of a heart attack, medical personnel attributed these readings to her pregnancy and dismissed her without the necessary follow-up. This oversight resulted in a preventable loss and has raised crucial questions about systemic healthcare inadequacies.
Unveiling the Flaws in Medical Diagnosis
Lack of Diagnostic Rigor and Its Consequences
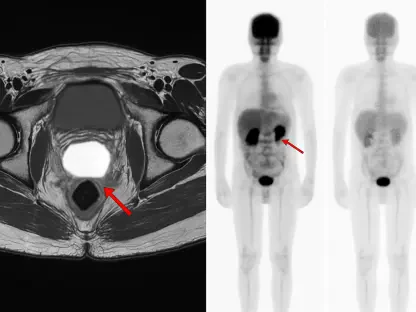
The incident involved key failures that highlighted the critical need for improved diagnostic protocols in medical institutions. Misidentification of heart attack symptoms in pregnant women like Ms. Kavanagh reveals an alarming gap in medical training and awareness. Typically, elevated Troponin levels serve as a red flag, signaling potential cardiac distress. Yet, in Ms. Kavanagh’s case, these signals were misinterpreted, and the potential risk was downplayed. Such medical misjudgments emphasize the need for healthcare providers to enhance diagnostic approaches, especially in complex cases involving confluences of conditions such as pregnancy and cardiac events.
Furthermore, this case underlines the importance of interdisciplinary collaboration in medical settings. When chest pains are presented by pregnant patients, multidisciplinary consultations could play a vital role, ensuring symptoms are thoroughly evaluated by specialists in both obstetrics and cardiology. The reliance on a singular interpretation of symptoms, without engaging comprehensive diagnostic resources, detracts from delivering safe and effective care. It stresses a pressing demand for hospitals to cultivate an environment of collaboration and comprehensive care.
Implications of Misdiagnosis in Maternal Healthcare
Misdiagnosis in the realm of maternal healthcare not only threatens the well-being of mothers and their unborn children but also contributes to a disheartening lack of trust in medical systems. Caroline Kavanagh’s case is a stark demonstration of how missteps in clinical judgment can devastate families. As expectant mothers entrust medical professionals with their care, they anticipate receiving thorough and attentive service. When these expectations falter, the ramifications are profound, affecting both the immediate circle of those impacted and the broader public view of healthcare proficiency.
The enduring legal battle faced by Kavanagh’s family underscores the slow pace of obtaining justice following medical errors. A decade-long pursuit for acknowledgment and reparation symbolizes not only the personal struggle of those indirectly bearing the consequences but also reflects on a judicial and healthcare system inadequately prepared to swiftly rectify such situations. The distress payment settled, although some economic recompense, pales in comparison to the irreparable emotional and familial loss suffered, underscoring the insufficiency of financial settlements alone as a form of reparative action.
A Decade-Long Wait for Acknowledgment and Justice
Evolving Legal and Health Care Systems
The legal journey endured by Caroline Kavanagh’s family reveals broader inadequacies within not just healthcare but also accompanying legal frameworks. After ten years, the family received an apology from Tipperary University Hospital and the HSE, expressing sympathy and acknowledging a failure in duty. However, this long-awaited admission of accountability indicates a systemic shortcoming in swiftly addressing and resolving instances of medical malpractice. It highlights a crucial need for structural reformations where timely acknowledgment and resolution are prioritized, thus fostering an environment where learning from failures institutes preventive measures.
Throughout this prolonged period, the family’s focus remained steadfastly on ensuring no other families face such preventable tragedies. Their case brought to light the pressing necessity for an overhaul in medical procedures, emphasizing accountability and enhanced patient safety. Implementing early corrective measures, matched with transparent communication, could be instrumental in not only preventing similar incidents but also in rebuilding public confidence in healthcare systems.
Future Steps Toward Safer Healthcare
Looking forward, creating a safer healthcare environment necessitates systemic change, encompassing not only better diagnostic practices but also prompt acknowledgment of errors. Establishing proactive training programs for medical professionals, prioritizing interdisciplinary cooperation, and fostering a culture of openness and responsibility are essential steps in this evolution. These reforms aim to develop a robust framework wherein instances of misdiagnosis become rare exceptions rather than recurring realities.
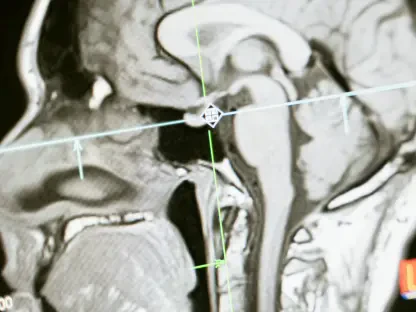
Furthermore, integrating technological advances, such as better diagnostic tools and predictive analytics, could aid practitioners in making informed decisions quickly. Rather than depending solely on subjective clinical interpretations, solutions involving technology could offer objective insights, thereby safeguarding against human error. As healthcare continues to evolve, the focus must shift towards patient-centered care, where both medical expertise and technological resources collectively ensure optimal outcomes.
Concluding Lessons and Steps Forward
The tragic case of Caroline Kavanagh and her unborn child at Tipperary University Hospital highlights the severe repercussions of diagnostic errors in healthcare. At 22 weeks pregnant, Ms. Kavanagh was hospitalized due to chest pains—a situation warranting thorough analysis given the delicate nature of her pregnancy. Unfortunately, a critical misjudgment occurred, failing to differentiate between symptoms associated with pregnancy and potential heart-related concerns. Elevated Troponin levels, typically suggestive of a heart attack, were mistakenly attributed to her pregnancy. Consequently, Ms. Kavanagh was discharged without the essential medical follow-up. This grievous oversight culminated in a life that could have been preserved, sparking significant inquiry into the broader systemic shortcomings in healthcare practices. Such incidents underscore the necessity for healthcare professionals to exercise diligence and precision, especially in pregnancies with concurrent health anomalies, to prevent similar tragedies in the future.