A patient’s chance of survival in a modern hospital often hinges not just on the skill of the medical staff, but on the reliability of the technology surrounding them. In Nigeria, a stark reality is unfolding within hospital wards where life-saving machines, from dialysis units to patient monitors, frequently lie dormant. This is not due to a lack of sophisticated equipment, but rather a systemic failure in its upkeep. The nation is grappling with what Minister of State for Health and Social Welfare, Dr. Iziaq Salako, recently described as a “poor maintenance culture,” a problem so pervasive that it threatens to undermine the very foundation of the country’s healthcare delivery system. In response, the government has launched a series of critical initiatives, including a comprehensive nationwide audit of high-end medical devices and a renewed focus on empowering the technical experts who are the last line of defense against technological decay. This pivotal moment raises a crucial question about whether these efforts can reverse decades of neglect and build a sustainable framework for medical technology management.
A Systemic Breakdown and the Government’s Response
Acknowledging a Deep-Rooted Problem
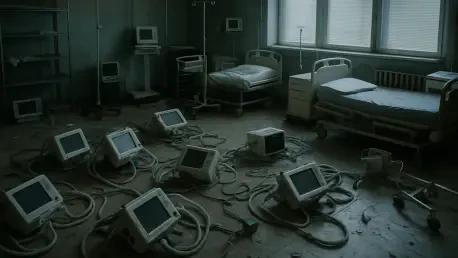
The deteriorating state of medical equipment across Nigerian healthcare facilities has been traced to a convergence of persistent issues that go far beyond simple neglect. At a recent capacity-building workshop in Abuja, officials identified weak partnerships between government agencies, private sector stakeholders, and healthcare institutions as a primary obstacle. This lack of collaboration has stifled the development of a cohesive national strategy for equipment lifecycle management. Compounding this issue is the absence of structured, continuous training programs for the biomedical engineers tasked with maintaining these complex devices. Without ongoing professional development, technicians are often ill-equipped to handle newer technologies or perform routine preventative maintenance, leading to a reactive cycle of breakdown and repair rather than a proactive system of upkeep. The result is a landscape where expensive, high-end diagnostic and therapeutic equipment is frequently underutilized or abandoned altogether, creating significant gaps in patient care and wasting valuable national resources invested in healthcare technology.
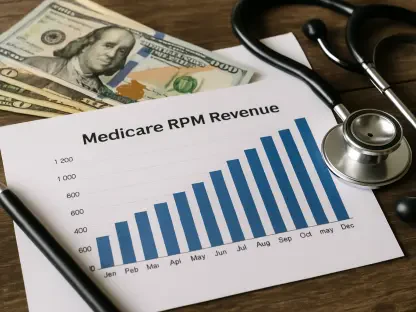
The government’s new strategy directly confronts these long-standing deficiencies through a multi-pronged approach under the broader Health Sector Renewal Investment Initiative. A central component of this plan is a comprehensive, nationwide audit of high-end medical equipment, designed to create an accurate inventory of existing technology and assess its functional status. This data will inform a more strategic allocation of resources for repair, replacement, and training. Simultaneously, the government is spearheading collaborative efforts like the five-day workshop for biomedical engineers, which brought together the ministry, Healthy Living Communications Ltd., and the College of Biomedical Engineering and Technology. The objective of such programs is to enhance the technical capacity of the healthcare workforce, ensuring they have the competence to maintain essential devices and minimize equipment downtime. Furthermore, the initiative includes plans to upgrade biomedical engineering schools and retrain existing staff, building a sustainable pipeline of skilled professionals who can act as “change agents” within their institutions, disseminating best practices and fostering a culture of diligent maintenance.
The Critical Role of Biomedical Engineers
The renewed national focus on healthcare infrastructure has cast a spotlight on the indispensable, yet often overlooked, role of biomedical engineers. Dr. Salako, represented by his Special Assistant Dr. Babatunde Akinyemi, emphasized that these professionals are the backbone of modern medical care, responsible for ensuring that the full spectrum of equipment—from diagnostic imaging machines to critical care ventilators—remains in optimal working condition. The COVID-19 pandemic served as a stark reminder of their importance, as the sudden, massive demand for ventilators and patient monitors highlighted how easily healthcare systems can collapse when technology fails. The most advanced medical devices are rendered useless without the expertise of engineers who can install, calibrate, maintain, and repair them. Their work directly impacts clinical outcomes by guaranteeing the accuracy of diagnostic tests, the efficacy of treatments, and the reliability of patient monitoring, making them a vital link in the chain of patient care. The government’s investment in their training is a direct acknowledgment that human capital is as crucial as the hardware itself.
This national initiative seeks to elevate the profession beyond its traditional boundaries, a transformation articulated by chief trainer Dr. Awafung Adie. He argued for a paradigm shift where biomedical personnel evolve from being perceived as mere “equipment repairers” to being recognized as integral healthcare technology managers, innovators, and leaders. This expanded role involves not just fixing broken machines but also participating in strategic planning, technology acquisition, and the development of institutional maintenance protocols. By empowering engineers to take on these responsibilities, Nigeria can begin to address the chronic issue of prolonged equipment downtime and reduce its heavy dependence on foreign technical support, which is often costly and slow to mobilize. This shift is crucial for building a self-reliant and resilient healthcare system. When biomedical engineers are integrated into leadership and decision-making processes, they can help ensure that technology is deployed and managed effectively, ultimately leading to improved patient safety and more efficient healthcare delivery across the country.
Perspectives from the Frontlines and Beyond
On-the-Ground Realities
The theoretical discussions about policy and strategy find their starkest validation in the firsthand accounts of those working within the Nigerian healthcare system. Chief Emmanuel Oriakhi of Healthy Living Communications Ltd. shared observations that paint a troubling picture of waste and missed opportunities. He recounted numerous instances of visiting hospitals only to find functional, sometimes relatively new, medical equipment abandoned in storerooms or corridors. The reason for their disuse was often not a catastrophic failure but a lack of routine maintenance or the absence of personnel with the updated knowledge required to operate or service them. This on-the-ground reality highlights a critical disconnect between procurement and lifecycle management. A significant investment is made in acquiring state-of-the-art technology, but the comparatively small, ongoing investment required for maintenance, software updates, and user training is frequently neglected. This pattern perpetuates a cycle where valuable assets depreciate rapidly, not from overuse, but from disuse, depriving countless patients of the advanced diagnostics and treatments they were intended to provide.
The International View and Patient Safety
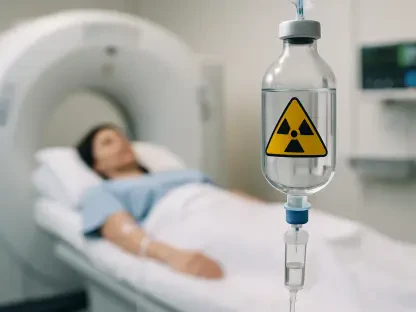
An international perspective offered by Mr. Dominiek Viaene, CEO of PROTEX Healthcare, brought the life-and-death consequences of this maintenance crisis into sharp focus. He drew a sobering comparison between the survival rates of dialysis patients in Nigeria and those in Europe, noting a significant disparity despite the fact that many hospitals in both regions use identical dialysis machines. This suggests that the discrepancy lies not in the quality of the technology itself, but in its maintenance and the procedural execution surrounding its use. When equipment is not properly calibrated or consistently serviced, its performance can degrade, leading to suboptimal treatments and, ultimately, poorer patient outcomes. This comparison serves as a powerful indictment of the current state of technical support within the Nigerian health sector, illustrating that possessing advanced medical equipment is only the first step. Without a robust and reliable system of maintenance and quality assurance, the potential of this technology to save lives remains tragically unfulfilled, turning a potential asset into a source of risk.
The issue extends beyond suboptimal performance into the realm of active patient harm. Mr. Viaene issued a stern warning against unsafe practices that have become alarmingly common in environments with poor technical oversight, such as the deliberate disabling of safety detectors on equipment. These safety features are designed to prevent catastrophic failures or alert clinicians to dangerous operating conditions. Bypassing them may seem like a quick fix to deal with a persistent alarm or a faulty sensor, but it is a reckless gamble that directly endangers patient lives. Such actions underscore a systemic breakdown in safety culture, one that can only be rectified through a concerted, collaborative effort. He called for a stronger alliance between the government, hospital administrators, and engineers to establish and enforce rigorous maintenance standards. Lasting improvement requires more than just training workshops; it demands the creation of sustained maintenance systems and a culture where patient safety is non-negotiable, ensuring that every piece of equipment is not only functional but also safe.
Forging a Path Toward Sustainable Healthcare Technology
The conversations and commitments that emerged from the recent initiatives marked a significant acknowledgment of the deep-seated challenges within Nigeria’s healthcare technology sector. The government’s audit and training programs represented a crucial first step, but the path forward required a fundamental cultural shift. It became clear that success depended not just on repairing machines, but on rebuilding the very framework that supports them. The consensus was that biomedical engineers had to be empowered as strategic managers, not just technicians, and integrated into every stage of the technology lifecycle, from procurement to decommissioning. Moreover, the stark warnings about patient safety and the disparities in clinical outcomes served as a powerful catalyst for change, highlighting that the true cost of neglect was measured in human lives. The proposed collaborations between public and private entities offered a promising model for creating a sustainable ecosystem where knowledge could be shared, standards could be enforced, and a culture of proactive maintenance could finally take root, potentially transforming the nation’s healthcare landscape for generations.