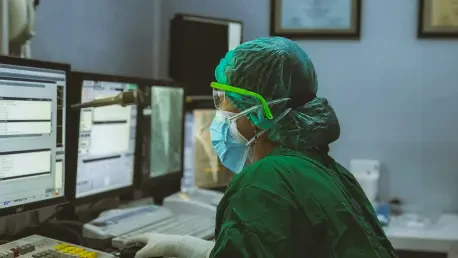
A deepening financial crisis is pushing American hospitals to the brink, forcing them into a precarious balancing act between fiscal survival and their fundamental mission of patient care. Caught between the relentless rise of operational costs and reimbursement rates that fail to keep pace, healthcare facilities across the nation are implementing drastic cost-cutting measures that were once considered unthinkable. These are not simple budgetary adjustments but profound shifts in operations that involve rationing essential supplies, delaying critical equipment upgrades, and altering patient care procedures. As administrators and clinicians navigate this unforgiving landscape, the situation raises an urgent and unsettling question about whether the struggle to remain financially solvent is quietly eroding the foundations of patient safety and compromising the quality of care that communities depend on. The daily compromises made in hallways and supply closets are becoming the new, unsettling norm in American healthcare.
The Financial Vise Grip
The core of the crisis lies in an unsustainable financial model where expenditures are dramatically outstripping revenues, creating a vise grip on hospital operations. In 2024 alone, hospital operating expenses surged by 5.1%, a figure that far exceeds the general inflation rate of 2.9%. The primary driver of this increase is the skyrocketing cost of labor, which now constitutes an overwhelming 56% of a hospital’s entire budget. This has been particularly exacerbated by a fierce competition for skilled professionals amid persistent labor shortages, causing wages for registered nurses to climb a staggering 26.6% above the general rate of inflation. This immense pressure on the largest portion of the budget leaves little room for absorption of other rising costs, forcing administrators to look for savings in areas that can directly impact the delivery of care. The financial strain is not a distant threat but an immediate reality that dictates the allocation of every dollar spent and every resource used within the hospital’s walls.
Compounding the problem of escalating expenses is the chronic inadequacy of reimbursement rates from both government and private payers. The revenue side of the ledger has failed to keep pace, creating a critical and growing gap. A stark illustration of this disparity comes from Medicare, which in 2023 covered only 83 cents for every dollar of care that hospitals provided, resulting in an estimated national shortfall of $130 billion in underpayments. This reimbursement gap has been widening for years; over a recent three-year period, general inflation grew by 14.1%, while Medicare reimbursement rates increased by a mere 5.1%. The rising prevalence of Medicare Advantage plans further intensifies this pressure. These plans typically pay out less than traditional Medicare and are associated with patient observation stays that are 37% longer, effectively shifting a greater financial and operational burden onto hospitals that are already struggling to manage their limited resources and maintain their standards of care.
A Brittle and Unreliable Supply Chain
Beyond the immediate financial pressures, hospitals are confronting an increasingly fragile and unpredictable medical supply chain that has transformed routine procurement into a high-stakes challenge. A deep-seated dependence on single-source suppliers for many critical items leaves healthcare facilities acutely vulnerable to disruptions caused by a wide range of factors, including natural disasters, international tariffs, and logistical bottlenecks. The catastrophic impact of such vulnerabilities was laid bare in 2024 when Hurricane Helene damaged a key IV fluid production plant, disrupting an astonishing 60% of the nation’s supply, with some facilities still struggling to recover from the fallout. This volatility has led to critical shortages of once-commonplace items, from IV tubing and sterile gloves to pediatric nebulizers and life-saving drugs like epinephrine. The result is a constant, resource-draining scramble for alternatives, turning what should be a predictable background process into a daily source of institutional anxiety and operational instability.
The consequences of this supply chain volatility are not abstract; they manifest in the day-to-day decisions made on hospital floors and in operating rooms across the country. Faced with dwindling inventories and uncertain delivery schedules, facilities are being forced to adopt “creative” but often undesirable workarounds. In a mid-sized Ohio hospital, a manufacturing delay for lidocaine IV bags threatened to halt scheduled surgeries until the pharmacy sourced an international version at nearly three times the standard price, converting a routine supply order into a major financial liability. Elsewhere, the reality is even more direct. A Michigan hospital supply room now uses stark color-coded labels to mark critically low supplies like saline flushes as “red,” while a California surgical team has begun modifying its procedure schedules to align with supply availability, prioritizing cases that require fewer consumables. These rationing tactics and procedural modifications are no longer hypothetical contingency plans but have become necessary, albeit uncomfortable, strategies for survival.
The Tangible Toll on Care and Infrastructure
The relentless financial and supply chain pressures are forcing hospitals to defer long-term investments in favor of meeting immediate operational needs, leading to a visible and potentially dangerous deterioration of physical infrastructure. With budgets consumed by unexpectedly high costs for basic supplies and inflated labor expenses, capital for upgrading or replacing aging equipment is often the first to be cut. In one Florida emergency department, staff are still using patient stretchers purchased in 2008, many of which now have cracked rails, because the funds allocated for their replacement were diverted to cover the rising price of generic antibiotics. This creates a perilous cycle where deteriorating infrastructure not only poses direct risks to patient safety but also hampers the efficiency of clinical staff who must work around faulty or outdated equipment. The postponement of these crucial investments is creating a hidden deficit in safety and quality that will have long-term consequences for patient care.
This environment of constant crisis places an immense burden on hospital staff, diverting their time and expertise away from patient care and toward logistical problem-solving. Pharmacists, for example, are now spending a significant portion of their workdays sourcing and validating alternative medications to navigate nationwide shortages, rather than focusing on their clinical duties. One facility’s staff had to test three different substitutes for an injectable steroid before finding one that met their clinical standards, accumulating substantial hidden labor costs in the process. While hospital leaders are actively working to build resilience through new strategies like forming regional purchasing networks or adopting AI-powered inventory systems, these solutions are not universally accessible. The high upfront cost of advanced technologies creates a growing disparity, leaving smaller, more financially vulnerable hospitals unable to afford the tools that could help them mitigate risk, widening the gap between the haves and the have-nots in healthcare resilience.
A System Stretched to Its Limit
The convergence of rampant cost inflation, inadequate reimbursement, and a brittle supply chain created a state of sustained duress for American hospitals. These institutions operated in an environment where basic stability could no longer be taken for granted, forcing compromises that were once unimaginable. While the healthcare system demonstrated remarkable ingenuity and resolve in adapting to this new reality, the myriad workarounds and stopgap measures proved to be temporary fixes, not long-term solutions. The unwavering dedication of healthcare professionals to patient care remained a constant, but the tools and resources needed to deliver that care became increasingly constrained. Ultimately, the challenge extended beyond the walls of any single hospital, posing a broader, more urgent question to policymakers and society about how to provide the systemic support necessary to relieve these essential institutions from a perpetual cycle of compromise and ensure their future viability.