A deeply concerning trend is quietly unfolding in examination rooms and radiology suites across the country, fundamentally altering the nature of medical documentation and the role of the physician. In what can only be described as a systemic usurpation of professional authority, external entities—ranging from hospital administrators and insurance companies to government regulators—are compelling doctors to insert pre-written, mandated text into the official medical record. This insidious practice, aptly termed “language laundering,” allows unqualified or unaccountable parties to practice medicine by proxy, using the physician’s hard-earned credentials as a shield for their own bureaucratic or financial agendas. This represents a profound violation of professional autonomy, forcing highly trained medical experts to sign their names to statements they did not author, effectively putting words in their mouths without their consent or expert agreement and shifting the landscape of medical liability in a perilous new direction.
The Core of the Conflict: Autonomy vs. Mandates
Undermining Professional Authority
The most fundamental grievance expressed by physicians is the systematic and escalating erosion of their authority over their own professional statements, which are the cornerstone of patient care. A particularly telling anecdote involves a radiologist who discovered that a simple software macro, one he used for years to streamline his workflow, had been covertly altered by a hospital administrator. Without his knowledge or consent, this change automatically inserted a lengthy, unvetted paragraph into every CT report he produced. This is not an isolated incident but a microcosm of a much larger, more pervasive pattern of intrusion. After dedicating more than a decade to rigorous education, enduring grueling residency programs, and making immense personal and financial sacrifices to earn their license, doctors justifiably feel a sense of outrage when non-physician personnel dictate the content of their expert medical evaluations. This practice effectively demotes them from trusted, autonomous authors of the medical narrative to mere scribes for a complex and often clinically detached bureaucratic machine.
This transformation of the physician’s role has profound implications for the integrity of the medical profession itself. When a doctor’s report is no longer a direct reflection of their expert analysis and judgment, its value is diminished. The process of medical evaluation, which should be a bespoke and nuanced assessment tailored to an individual patient, becomes a standardized, compliance-focused exercise in box-checking. The physician is no longer just a conduit for medical knowledge but a conduit for externally imposed language that may have little to no clinical relevance. This not only devalues their expertise but also creates a dangerous precedent where administrative requirements or financial incentives can override sound medical practice. The very act of being forced to “parrot” language one did not write compromises the ethical foundation of medicine, turning a sacred doctor-patient document into a tool for institutional or corporate objectives, a shift that ultimately undermines the trust placed in physicians by both their patients and their referring colleagues.
The Accountability Shell Game
The metaphor of “language laundering” brilliantly captures the alarming lack of accountability at the very heart of this issue, drawing a parallel to the criminal act of concealing the origins of illicit funds. In a similar vein, external groups effectively wash their unqualified mandates and bureaucratic directives through the credibility of a physician’s report. A hospital administrator, an insurance clerk, or a government regulator cannot legally or ethically author a medical document that dictates patient care. However, by coercing or compelling a licensed doctor to include their pre-approved text, that language becomes legitimized, carrying the full legal and professional weight of the doctor’s name and credentials. This allows these interlopers to influence medical practice and documentation from the shadows, effectively practicing a form of medicine by proxy without ever holding a medical license or being directly answerable for the clinical implications of their words. It is a sophisticated end-run around the established legal and ethical frameworks designed to protect patients from unqualified practitioners.
The most critical and dangerous flaw in this system is the deliberate and complete transfer of liability. When this mandated text—whether it’s an ambiguous phrase inserted for billing purposes or a legally protective clause required by risk management—leads to patient harm, a misdiagnosis, or a subsequent lawsuit, the legal and professional responsibility falls squarely and solely on the physician whose signature is at the bottom of the report. The administrative committee, the insurance company’s policy department, or the government agency that created the text remains entirely shielded from accountability. This creates a fundamentally unjust and perilous imbalance where the originators of the language bear no risk for its consequences, while the medical professional who may have had no control over its inclusion assumes all of it. This accountability shell game not only puts physicians in an untenable position but also poses a significant, hidden threat to patient safety by prioritizing compliance and risk mitigation over clear, accurate, and unencumbered medical communication.
The Web of Influence: Sources and Consequences
Identifying the Interlopers
The pressure on physicians to cede control over their medical reports comes from a wide and varied array of sources, which can be collectively described as “interlopers” in the clinical process. Prominent among these are hospital and practice administrators, who frequently impose standardized text to ensure compliance with internal policies or complex external incentive programs like the Merit-based Incentive Payment System (MIPS). Their motives are often driven by institutional metrics and financial performance rather than the nuances of individual patient care. Equally influential are third-party payors, particularly insurance companies, which are notorious for inserting language specifically designed to streamline billing processes or, more cynically, to create grounds for claim denials. This corporate-driven verbiage often adds clutter and ambiguity, serving the insurer’s bottom line at the direct expense of clinical clarity and the physician-patient relationship, forcing doctors to become unwilling participants in the financial machinery of healthcare.
The web of influence extends far beyond the confines of the hospital and the insurance industry, reaching into the halls of government and the legal departments of healthcare institutions. Government bodies, politicians, and their associated regulatory agencies create and enforce reporting requirements through legislation and mandates, compelling physicians to include specific phrases or data points that serve public health goals or regulatory oversight. While often well-intentioned, these requirements can be rigid and may not apply uniformly to every clinical scenario. Furthermore, institutional risk management departments have become a significant source of mandated language, requiring doctors to insert carefully crafted phrasing intended to mitigate legal exposure for the hospital. This defensive medicine, practiced through documentation, prioritizes legal protection over clear communication. Even historically respected medical organizations have inadvertently contributed to this trend; systems like the Breast Imaging Reporting and Data System (BI-RADS), despite their undeniable clinical value, set an early and powerful precedent for an external body dictating the precise structure and wording of a physician’s findings.
The Clinical and Professional Fallout
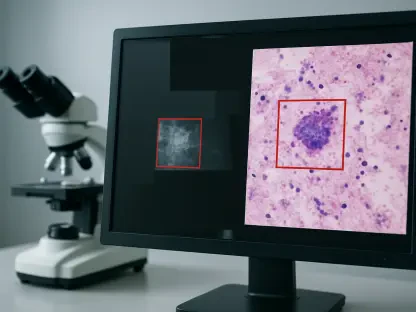
The most immediate and tangible clinical consequence of this widespread practice is the phenomenon of “report bloat.” Medical reports, once concise and direct summaries of a physician’s findings, are now frequently cluttered with lengthy, boilerplate paragraphs of non-essential, mandated information. This extraneous text often buries the key diagnostic findings and actionable recommendations deep within a wall of administrative and legal jargon. As a result, referring clinicians, who are already facing immense time pressures, are forced to waste precious minutes sifting through this irrelevant fluff to locate the critical data needed to make timely and informed treatment decisions. This not only introduces inefficiency into the healthcare system but also significantly increases the risk of confusion and medical error. When crucial information is obscured by bureaucratic language, the potential for misinterpretation or oversight grows, posing a direct threat to patient safety and the quality of care.
Beyond the clinical risks, this practice inflicts a significant professional and ethical toll on physicians, leading to a palpable erosion of their professional integrity. Being compelled to “parrot” statements they did not author, and with which they may not fully agree, fundamentally compromises their role as independent, expert evaluators. The act of affixing their signature to a document that is less a bespoke medical analysis and more a patchwork of compliance-driven text turns a deeply personal and professional responsibility into a hollow administrative task. This forces doctors into an ethical quandary, where they must lend their expert authority to language that may not accurately reflect their nuanced medical judgment. Over time, this can lead to burnout, demoralization, and a growing sense of disillusionment with a system that appears to value bureaucratic conformity over the physician’s expertise, ultimately weakening the very foundation of trust and autonomy upon which the medical profession is built.
A Call for Transparency and Rebellion
In the face of this deeply entrenched problem, a dialogue emerged around potential solutions, ranging from the practical to the openly rebellious, all aimed at reclaiming the integrity of the medical report. Technologically, it was recognized that modern reporting systems, perhaps enhanced with the help of artificial intelligence, could have been designed to offer functionalities that isolate or allow a referring physician to “hide” all non-doctor-generated content. Such a feature would have empowered clinicians to view a clean, concise report containing only the essential medical findings, free from the clutter of administrative and legal boilerplate. More pointedly, a fantasy of professional defiance took shape, imagining physicians adding a blunt and transparent disclaimer at the end of their reports: “My official dictated report ends here. Below please find statements which have been required by my employer and licensing/credentialing authorities, over which I have no control.” While it was understood that such an act would likely have labeled a doctor as a troublemaker, the potential satisfaction of reclaiming one’s professional voice and restoring honesty to the medical record highlighted the profound frustration that drove the desire for meaningful change and a return to physician-led documentation.