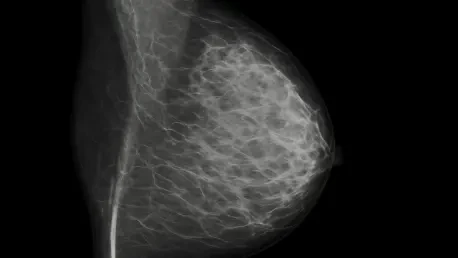
When a mammogram flags a concern, the clock starts ticking on follow-up care that too often stalls in confusion, voicemail loops, and missed appointments that undermine early detection. That gap—by SimonMed’s estimate, missed by up to 30% of eligible patients—has become the target of a new mobile-first, HIPAA-compliant platform designed to turn screening results into clear next steps. Instead of expecting patients to decode radiology jargon or navigate fragmented portals, the system translates findings into plain language, highlights urgency, and personalizes guidance. It ties into SimonMed’s AI-enhanced Mammogram+ program, using breast density, lifetime risk scores, and other clinical signals to tailor recommendations. The experience resembles consumer apps not in gloss, but in utility: short explainer videos, a conversational AI health guide, and access to a human navigator for scheduling and questions, all engineered to convert intent into action.
How the platform reshapes follow-up pathways
At the center is Cascaid Health’s clinical-grade AI, which synthesizes imaging insights with risk models to suggest evidence-based next steps, from diagnostic views and ultrasound to MRI referrals and specialist consults. Rather than simply alerting a patient that something looked “inconclusive,” the platform contextualizes why density matters, how risk is calculated, and what timing is recommended. Moreover, it syncs with referring providers so primary care teams receive integrated updates instead of disconnected faxes, tightening the loop between radiology, clinicians, and patients. The goal is less about novelty than adherence: by clarifying rationale and offering immediate scheduling, the system aims to boost completion rates for timely follow-up imaging, especially among women with dense breasts or elevated risk profiles. In contrast to standalone portals, it treats navigation, education, and coordination as a single workflow.
What adoption could mean next
The launch pointed to a practical shift: using AI not only to interpret images, but to manage the last mile of care where delays often occur. Early impact data remained to be independently verified, yet the design centered on measurable outcomes such as completed appointments within recommended windows and reduced no-shows after high-risk screens. To scale, payers and health systems would have pursued alignment on quality measures, while radiology groups considered interoperability, language access, and equity for patients without stable broadband. The most promising extensions involved embedding decision support into primary care visits, automating reminders keyed to risk, and closing feedback loops when results cleared concerns. If those steps held, the platform would have advanced adherence while giving providers a cleaner line of sight into follow-up—and patients a clearer path from uncertainty to resolution.