A groundbreaking five-year retrospective study has provided compelling evidence that an advanced imaging technique is revolutionizing the management of recurrent prostate cancer. Researchers have demonstrated that prostate-specific membrane antigen (PSMA) PET/CT scans offer a highly sensitive tool for pinpointing the exact location of cancer cells after surgery, a capability that eludes conventional imaging methods. This newfound clarity allows physicians to personalize and more accurately target radiation therapy, leading to significantly improved long-term outcomes. The findings signal a major shift away from standardized treatment protocols, promising a future where therapy is more effective and patients are spared the debilitating side effects of overly aggressive or unnecessary interventions. For the substantial number of men who face a cancer recurrence, this imaging technology represents a pivotal advancement in their therapeutic journey.
A New Lens on Recurrent Cancer
The primary challenge in managing biochemical recurrence, which affects up to 40% of men within a decade of a prostatectomy, has long been diagnostic uncertainty. A rising prostate-specific antigen (PSA) level indicates cancer is present, but traditional imaging modalities such as bone scans, CT, and MRI are often not sensitive enough to detect the source, especially at the very low PSA levels where intervention is most effective. This lack of precision has historically forced clinicians into a one-size-fits-all strategy involving salvage radiation therapy. This approach often entails irradiating broad areas, including the entire prostate bed and pelvic lymph nodes, and sometimes adding systemic hormone therapy (androgen deprivation therapy) as a precaution. While beneficial for some, this standardized protocol can expose many men to treatments they do not need, along with significant side effects that can diminish their quality of life, without a clear understanding of where the recurrent disease is actually located.
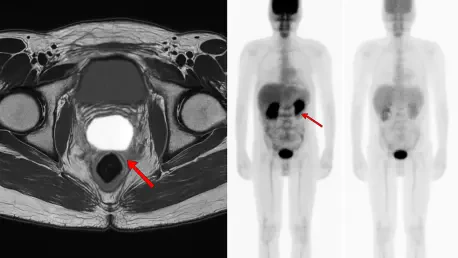
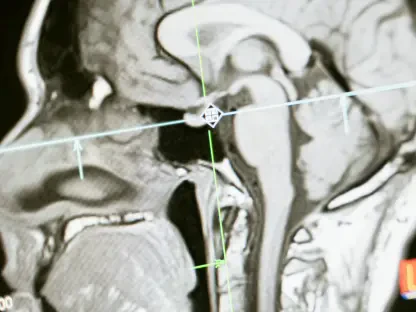
The transformative potential of PSMA PET/CT imaging lies in its fundamentally different mechanism. This advanced diagnostic tool utilizes a unique radioactive tracer meticulously designed to bind to the prostate-specific membrane antigen, a protein that is heavily overexpressed on the surface of most prostate cancer cells. This targeted binding process allows the scan to illuminate even minuscule clusters of malignant cells that would remain completely invisible on standard scans. The result is a clear and precise map of the recurrent disease, providing clinicians with invaluable information. It reveals whether the cancer is confined to the original prostate bed, has migrated to nearby pelvic lymph nodes, has metastasized to distant sites like bones, or is not yet detectable. This detailed anatomical information provides an unprecedented level of insight, forming the basis for a truly personalized treatment strategy that moves far beyond the limitations of older technologies.
Tailoring Treatment with Precision Imaging
Armed with the detailed map provided by a PSMA PET/CT scan, oncologists can pivot from a generalized treatment plan to a highly individualized therapeutic approach. The comprehensive study meticulously documented how this precise imaging directly informed critical clinical decisions that were tailored to each patient’s unique disease presentation. For instance, the scan results guided the determination of the radiation field, helping physicians decide whether to limit treatment to the prostate bed or expand it to encompass the whole pelvis. It also enabled the use of dose escalation, a technique where a higher, more potent dose of radiation is delivered directly to tumors made visible by the scan. Furthermore, the decision to add androgen deprivation therapy, a treatment with considerable side effects, was no longer a default but a targeted choice reserved for patients where imaging confirmed the cancer had spread, ensuring that only those who would truly benefit received it.
The long-term analysis of the 113 men who participated in the study yielded definitive findings that underscore the clinical utility of this imaging-guided paradigm. Patients whose scans showed cancer localized solely to the prostate bed or nearby pelvic lymph nodes derived the most significant benefit from receiving whole-pelvis radiotherapy, which treats both the prostate bed and the adjacent lymph node chains. In contrast, the addition of androgen deprivation therapy was shown to produce superior outcomes specifically for patients whose scans confirmed the cancer had spread to lymph nodes or distant sites. This allows for the judicious use of hormone therapy, sparing many men from its side effects. Perhaps most reassuringly, men whose PSMA PET/CT scans showed no visible signs of disease had the best overall outcomes, suggesting that for this subgroup, early and standard salvage radiation directed at the prostate bed is a highly effective standalone treatment.
An Imaging-Based Future for Patient Care
After five years of follow-up, the patient outcomes reported in the study were overwhelmingly positive. The data revealed that nearly all participants were still alive, and an impressive 72% had not experienced any distant spread of their cancer, a testament to the efficacy of the personalized treatments. A particularly crucial observation was that traditional clinical markers, such as the specific PSA level at the time of treatment, did not strongly correlate with the long-term response to the therapy. This finding highlighted a pressing need to evolve clinical practice, shifting from decisions based primarily on blood markers to a more refined, imaging-based paradigm for personalizing patient care. The study’s conclusions strongly supported the integration of PSMA PET/CT results into clinical guidelines, heralding a new standard of care where treatment for recurrent prostate cancer could be more effective, better targeted, and customized to the unique circumstances of each individual.