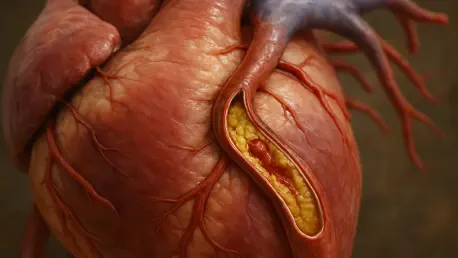
In a world where coronary artery disease (CAD) remains a leading cause of heart-related illness and death, the emergence of photon-counting computed tomography (PCD-CT) offers a transformative approach to early detection and management. This condition, defined by the narrowing of arteries due to plaque buildup, often manifests as persistent chest pain and can escalate into life-threatening events if not addressed promptly. While traditional imaging techniques like energy-integrating detector CT (EID-CT) have long been relied upon for non-invasive diagnosis, their limitations in precision have left room for improvement. A recent study published in European Radiology highlights how PCD-CT delivers a significant leap in diagnostic accuracy, potentially reducing the reliance on invasive procedures and paving the way for better patient outcomes. This advancement signals a shift in how clinicians might approach CAD, focusing on both enhanced detection and streamlined care.
Advancements in Diagnostic Technology
Superior Imaging Capabilities
The introduction of PCD-CT marks a notable departure from the capabilities of traditional EID-CT, particularly in detecting the extent of artery narrowing in patients with suspected CAD. In a comprehensive study involving 252 individuals experiencing stable chest pain, researchers found that PCD-CT consistently surpassed EID-CT across multiple evaluation metrics. Specifically, for blockages exceeding 70 percent, PCD-CT achieved an impressive accuracy of 90.9 percent at the patient level compared to EID-CT’s 70.6 percent. At the vessel level, the accuracy stood at 94.6 percent versus 80.9 percent, and at the segment level, it reached 98.6 percent against 94.1 percent. This enhanced precision stems from PCD-CT’s ability to capture finer details of arterial structures, enabling a clearer distinction of critical obstructions that require immediate attention. Such advancements suggest that this technology could redefine diagnostic standards by providing a more reliable foundation for clinical decisions.
Expert Validation of Performance
Insights from leading researchers further underscore the potential of PCD-CT to transform cardiac imaging, especially for those with stable angina. Melissa Boussoussou, M.D., Ph.D., from Semmelweis University Heart and Vascular Center in Budapest, Hungary, emphasized the technology’s exceptional performance at both vessel and segment levels during coronary CT angiography assessments. This granular accuracy means that clinicians can pinpoint the exact location and severity of blockages with greater confidence, which is crucial for tailoring individualized treatment plans. Unlike broader assessments that might miss subtle yet significant issues, PCD-CT offers a detailed view that could prevent misdiagnosis and unnecessary interventions. The expert endorsement highlights a growing consensus that this imaging tool may soon become a cornerstone in non-invasive diagnostics, setting a new benchmark for evaluating coronary health in clinical settings.
Impact on Patient Care and Procedures
Minimizing Invasive Interventions
One of the most promising aspects of PCD-CT lies in its potential to significantly reduce the need for invasive coronary angiography (ICA), a procedure often associated with risks such as bleeding or infection. Utilizing a Monte Carlo simulation model, the study projected a 14.8 percent decrease in ICA referrals for patients evaluated with PCD-CT compared to those assessed with EID-CT. This translates to fewer unnecessary procedures—approximately 821.7 referrals with PCD-CT versus 964.3 with EID-CT after extensive iterations. The reduction is largely due to the technology’s ability to minimize false positives, ensuring that only patients with confirmed severe blockages are directed toward invasive testing. By offering a more accurate non-invasive alternative, PCD-CT not only enhances patient safety but also alleviates the procedural burden on individuals who might otherwise undergo risky and avoidable interventions.
Streamlining Healthcare Delivery
Beyond individual benefits, the adoption of PCD-CT holds the potential to optimize resource allocation within healthcare systems facing constant pressure. Fewer referrals for invasive procedures mean reduced demand on catheterization labs, shorter wait times for patients requiring urgent care, and a lighter workload for radiologists and cardiologists. This efficiency could also translate into lower healthcare costs, as resources are directed more precisely toward those in critical need rather than spread thinly across unnecessary tests. The shift toward non-invasive diagnostics aligns with a broader movement in medicine to prioritize patient safety and operational effectiveness. As hospitals and clinics grapple with high patient volumes, integrating such technology could create a more sustainable model of care, ensuring that limited resources are used where they matter most while maintaining high diagnostic standards.
Challenges and Future Directions
Overcoming Study Constraints
Despite the encouraging findings surrounding PCD-CT, certain limitations in the current research must be acknowledged to ensure its broader applicability. The study, while robust with 252 participants across multiple centers, represents a relatively modest sample size that may not fully reflect the diversity of CAD patients globally. Variations in demographics, disease severity, and comorbidities could influence outcomes in ways not captured by this cohort. Additionally, the lack of long-term data on patient outcomes following PCD-CT diagnosis raises questions about its sustained impact over time. Expanding research to include larger, more varied populations will be essential to validate these initial results. Only through such efforts can the medical community gain a comprehensive understanding of how this technology performs across different contexts and patient groups, ensuring its reliability as a diagnostic tool.
Standardizing Protocols for Wider Use
Another critical challenge lies in the absence of standardized protocols for ultra-high-resolution imaging with PCD-CT, which could hinder its integration into routine clinical practice. Without uniform guidelines, results may vary between facilities, undermining consistency and trust in the technology. Furthermore, the study did not provide a quantitative comparison with ICA, leaving some uncertainty about how PCD-CT measures up in all diagnostic scenarios. Future research should prioritize establishing clear imaging standards and exploring the cost-effectiveness of widespread adoption. Assessing long-term benefits, such as reduced healthcare expenditures and improved patient prognosis, will also be vital. As efforts continue to address these gaps, the path forward involves collaboration among researchers, clinicians, and policymakers to ensure that PCD-CT can deliver on its promise as a game-changer in managing coronary artery disease effectively.
Reflecting on a Diagnostic Breakthrough
Looking back, the exploration of photon-counting CT through the lens of a pivotal study in European Radiology revealed a remarkable stride in combating coronary artery disease. Its superior accuracy, with gains of over 20 percent at the patient level for severe blockages, redefined expectations for non-invasive imaging. The projected reduction in invasive procedure referrals by nearly 15 percent underscored a tangible shift toward safer patient experiences and more efficient healthcare systems. Though challenges like limited sample diversity and unstandardized protocols persisted, the groundwork laid by this research pointed to a transformative era in cardiac care. Moving forward, the focus should shift to expanding studies, refining guidelines, and evaluating economic impacts to solidify PCD-CT’s role. Such steps will ensure that this technology evolves from a promising innovation into a widely accessible solution, ultimately enhancing the way clinicians diagnose and manage heart conditions.