A fundamental transformation is reshaping the medical landscape as diagnostic data evolves from a collection of static, historical results into a dynamic stream of real-time biological signals essential for the future of healthcare. This evolution is being driven by the rise of “diagnostic intelligence,” a strategic framework that combines real-time diagnostic information with advanced analytics and clear clinical policies to foster more precise, proactive, and personalized medical decisions. According to analysis from Dr. Bill Kerr, this new paradigm is not merely an incremental improvement but a foundational shift that positions diagnostic data as the central and most powerful asset in the modern healthcare ecosystem. As the industry continues its transition toward value-based care (VBC) and precision medicine, the ability to harness these insights is becoming the critical determinant of both clinical and financial success, promising a future where treatment is guided by a deep understanding of each patient’s unique biological makeup.
The Predictive Edge of Modern Diagnostics
The assertion that diagnostic data is poised to become healthcare’s most valuable IT resource stems from its unique, forward-looking nature. A sharp distinction exists between this class of information and more traditional health IT assets, such as claims or Electronic Health Record (EHR) data. While EHR and claims data are inherently retrospective, documenting clinical events and transactions that have already occurred, diagnostic data offers an unprecedented real-time window into a patient’s active biological processes. This allows clinicians to understand what is happening at a molecular or cellular level, often long before physical symptoms manifest. This capability provides a powerful predictive advantage, enabling interventions that can alter the course of a disease rather than just manage its consequences. This shift from a reactive to a proactive stance is a cornerstone of next-generation healthcare delivery.
This transformative power is fueled by the rapid proliferation of advanced diagnostic tools that are redefining the boundaries of medical science. Innovations including comprehensive genetic testing, sensitive biomarkers, polygenic risk scores, liquid biopsies, and blood-based markers for neurodegenerative diseases like Alzheimer’s are providing an unparalleled depth of insight. These technologies unlock information about an individual’s disease risk, the likely progression of their condition, and their probable response to specific treatments. By providing this granular, forward-looking intelligence, these tools are fundamentally changing the healthcare paradigm. The focus is no longer solely on treating established illnesses but on actively preventing them, detecting them at their earliest and most treatable stages, and personalizing care with a level of precision that was previously unattainable.
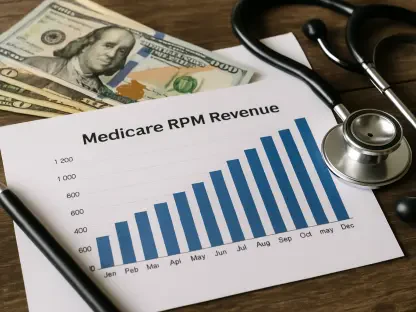
Fueling the Next Wave of Value-Based Care
The next evolution of value-based care will be heavily reliant on the advanced insights provided by diagnostic intelligence. The primary goal of VBC—to achieve superior patient outcomes while simultaneously reducing unnecessary costs—is directly supported by this data-driven approach. When clinicians are equipped with tools that clarify a patient’s unique biology, they can intervene earlier and with far greater confidence. This capability facilitates the selection of therapies with a high probability of success, thereby avoiding the costly, lengthy, and often frustrating process of trial-and-error that has historically characterized the management of many complex diseases. This move toward scientifically guided therapy selection is essential for delivering on the promise of VBC, ensuring that resources are directed toward interventions that provide the most significant clinical benefit for each individual patient.
In an era defined by the rise of expensive specialty drugs and targeted therapies, diagnostic intelligence also serves as a crucial safeguard for both patients and the healthcare system. It ensures that these powerful and costly treatments are correctly matched to the patients who will actually benefit from them. By identifying the specific molecular or genetic markers that a therapy targets, diagnostics prevent the administration of ineffective treatments, which not only represent significant financial waste but can also expose patients to unnecessary side effects and delay access to more appropriate care. This gatekeeping function is vital for maintaining the financial sustainability of precision medicine and ensuring that its revolutionary potential is realized responsibly, preventing potential harm and maximizing the value of every healthcare dollar spent.
Overcoming Deep-Seated Systemic Inefficiencies
Diagnostic intelligence is proving to be a powerful instrument for overcoming the persistent operational barriers that have long hindered the widespread adoption of personalized care within VBC models. Systemic issues, such as inconsistent utilization of essential tests, critical delays in obtaining certain biopsy results, and uneven adherence to evidence-based clinical guidelines, have created significant clinical variation. This variability not only drives up costs through redundant or unnecessary procedures but can also lead to suboptimal patient outcomes. These entrenched inefficiencies have traditionally been difficult to identify and address, often hidden within complex clinical workflows and disparate data systems, making standardized, high-quality care a challenging goal to achieve at scale.
By applying a layer of advanced analytics to the vast streams of diagnostic data, health systems, providers, and health plans can now identify these gaps and inefficiencies in real time. This data-driven oversight facilitates the implementation of more consistent, standardized, and evidence-based clinical practices across an entire organization. In this context, diagnostics are transformed from a back-end cost center into a frontline, strategic asset that actively reduces waste and ensures the right care is delivered to the right patient at the right time. This strategic application of diagnostic intelligence allows healthcare organizations to proactively manage care pathways, optimize resource allocation, and drive continuous quality improvement, thereby strengthening the operational foundation required for successful value-based care delivery.
Paving the Way for a Smarter Healthcare System
The synthesis of diagnostic data with artificial intelligence and advanced analytics became a critical enabler of smarter treatment decisions. These integrated systems revealed complex patterns in imaging and laboratory data that might have been missed by traditional methods, which in turn enhanced the clarity needed to monitor disease progression and inform crucial clinical choices. As healthcare costs continued to rise, this level of precision became essential for achieving financial sustainability and optimal patient care. The exponential growth in data from advanced testing fed and improved predictive models, which led to the refinement of clinical guidelines and decision-support tools. This virtuous feedback loop extended the benefits of precision medicine beyond specialized care into broader applications like chronic disease management and population health initiatives, laying the groundwork for a continuously learning healthcare ecosystem. This analytical power also highlighted how diagnostic data could be used to advance health equity, as the analysis of testing and treatment patterns across different populations identified disparities and enabled focused interventions to close critical gaps in care.