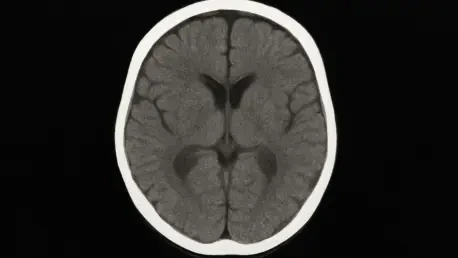
In an era where medical imaging has transformed pediatric care, brain CT scans stand out as a vital tool for diagnosing serious conditions like head trauma and cancer in children. Yet, beneath their undeniable benefits lies a troubling concern: the exposure to ionizing radiation, particularly its impact on delicate structures such as the eye lens, raises significant questions about long-term safety. With the rising frequency of these scans in young patients, parents, healthcare providers, and researchers alike are grappling with the challenge of ensuring that the diagnostic power of CT scans does not compromise the future health of children. This article explores the risks associated with radiation exposure during pediatric brain imaging, delving into the vulnerabilities of young patients, the inconsistencies in safety practices, and the potential solutions that could safeguard eye health without sacrificing critical diagnostic capabilities.
The stakes are high when it comes to radiation exposure in children, as their developing bodies are far more sensitive to potential damage than those of adults. The eye lens, in particular, is prone to harm from even small doses of radiation, which can accumulate over time and increase the risk of cataracts later in life. Many pediatric patients undergo multiple scans for ongoing conditions, amplifying the concern about cumulative exposure. This reality prompts a deeper examination of whether current imaging practices strike an appropriate balance between immediate diagnostic needs and the protection of long-term well-being, especially for the most vulnerable.
Understanding Radiation Risks in Pediatric Imaging
The Vulnerability of Young Eyes
The heightened sensitivity of children to ionizing radiation sets them apart from adults, making pediatric brain CT scans a topic of significant concern. Unlike fully developed tissues, the cells in a child’s body are rapidly dividing, which increases the likelihood of radiation-induced damage. The eye lens, a critical and radiosensitive structure, is particularly at risk during brain scans due to its proximity to the scanned area. Research indicates that even low levels of radiation exposure can initiate cellular changes in the lens, potentially leading to cataract formation years down the line. This vulnerability underscores why minimizing exposure is not just a precaution but a necessity in pediatric care, as the consequences may not manifest until much later in life, long after the initial scans are performed.
Beyond the immediate biological risks, the frequency of imaging in pediatric patients adds another layer of complexity to the issue. Children with chronic conditions, such as cancer or neurological disorders, often require repeated CT scans to monitor their progress or detect complications. Each scan contributes to a cumulative radiation dose, heightening the potential for long-term eye damage. While the diagnostic benefits of these scans are often life-saving, the lack of precise thresholds for safe exposure levels leaves medical professionals and families in a difficult position. Addressing this challenge requires not only awareness of the inherent risks but also a commitment to exploring every possible avenue to reduce unnecessary radiation while still ensuring accurate diagnoses.
Long-Term Implications of Early Exposure
The long-term implications of radiation exposure during childhood are a pressing concern for both medical experts and families. Cataracts, a well-documented outcome of radiation damage to the eye lens, can severely impair vision and quality of life if they develop as a result of early exposure. Studies have shown that the risk is not merely theoretical but quantifiable, with even small doses contributing to cellular changes over time. For children who undergo brain CT scans at a young age, the latency period before symptoms appear means that the full impact may not be evident until adulthood, making it challenging to gauge the true extent of harm in the short term. This delayed effect calls for a proactive approach to safety that prioritizes prevention over reaction.
Compounding this issue is the uncertainty surrounding individual responses to radiation. Not every child exposed to the same dose will experience identical outcomes, as genetic factors and overall health play a role in determining susceptibility. This variability complicates efforts to establish universal safety guidelines, leaving room for debate about how much exposure is acceptable. Furthermore, the psychological burden on families cannot be ignored, as the fear of potential health issues looms large even when immediate results are reassuring. Tackling these long-term implications demands a multifaceted strategy that includes ongoing research into radiation effects, better risk communication, and tailored approaches to imaging that account for each patient’s unique circumstances.
Challenges in Standardizing Safety Protocols
Variability in Exposure and Inconsistent Practices
One of the most significant hurdles in ensuring the safety of pediatric brain CT scans is the wide variability in radiation doses delivered across different medical facilities. Factors such as the type of CT machine, specific scan settings, and adherence to institutional protocols can result in substantial differences in the amount of radiation reaching the eye lens. In some cases, outdated equipment or suboptimal settings lead to higher exposure levels than necessary, while other facilities may employ advanced dose-reduction techniques. This lack of uniformity means that two children undergoing similar scans in different hospitals could face vastly different risks, highlighting a critical gap in standardized safety measures that needs urgent attention from the medical community.
Equally concerning is the inconsistency in how safety practices are applied by healthcare providers. While some institutions strictly follow guidelines to minimize radiation exposure, others may lack the resources or awareness to implement such measures effectively. This disparity often stems from variations in training and access to updated technology, leaving certain pediatric patients more vulnerable to unnecessary risks. The absence of a cohesive framework for radiation safety in imaging underscores the need for systemic change, including mandatory protocols that ensure every facility prioritizes dose optimization. Until such standardization is achieved, the potential for preventable harm remains a persistent challenge in pediatric radiology.
Gaps in Professional Awareness and Training
A deeper issue contributing to inconsistent safety practices is the gap in awareness among healthcare professionals about the risks of radiation exposure during pediatric CT scans. Many providers, while skilled in diagnostics, may not fully understand the long-term implications of repeated imaging on sensitive structures like the eye lens. This knowledge deficit can lead to decisions that prioritize speed or image clarity over minimizing dose levels, inadvertently increasing risks for young patients. Addressing this gap requires a concerted effort to integrate radiation safety into medical training curricula, ensuring that all practitioners are equipped with the latest information on best practices for pediatric imaging.
Moreover, ongoing professional development plays a crucial role in bridging this awareness gap. As imaging technology evolves, so too must the education provided to radiologists and other medical staff. Workshops, certifications, and regular updates on dose-reduction techniques can empower providers to make informed choices that balance diagnostic accuracy with patient safety. Without such initiatives, the risk of overexposure due to outdated practices or simple oversight remains high. The medical field must also foster a culture of accountability, where questioning and refining imaging protocols becomes standard, ultimately protecting children from avoidable harm through a commitment to continuous learning and improvement.
Exploring Solutions for Safer Imaging
Education, Alternatives, and Policy Reform
Enhancing education for healthcare professionals stands as a cornerstone for improving safety in pediatric brain CT scans. Many providers lack comprehensive training on the specific risks of radiation exposure to children, particularly to vulnerable areas like the eye lens. Implementing mandatory courses and regular updates on dose optimization techniques can address this shortfall, ensuring that medical staff are well-versed in minimizing exposure without compromising diagnostic quality. Additionally, fostering collaboration between radiologists and pediatric specialists can lead to tailored imaging plans that prioritize safety. Empowering professionals with knowledge is a critical step toward reducing risks and building trust with families who rely on their expertise for their children’s care.
Another promising avenue for safer imaging lies in the use of alternative modalities like magnetic resonance imaging (MRI), which avoids ionizing radiation entirely. While MRI cannot replace CT scans in all scenarios—particularly in emergencies due to longer scan times and limited availability—it offers a viable option for non-urgent cases. Encouraging the use of MRI when feasible can significantly lower radiation risks, especially for children requiring frequent imaging. However, barriers such as cost and accessibility must be addressed to make this alternative more widely adopted. Policymakers and healthcare leaders should work to improve access to MRI technology, ensuring that safer options are within reach for more patients and reducing reliance on radiation-based scans.
Lastly, policy reform at both institutional and governmental levels is essential to enforce consistent safety standards. Developing universal guidelines for pediatric CT protocols, including mandatory dose reporting and the use of protective measures like lead shields, can minimize exposure to the eye lens. Engaging parents in the decision-making process through informed consent discussions about radiation risks and alternatives also fosters a culture of advocacy for children’s safety. Stronger regulations, combined with public awareness campaigns, can drive systemic change, ensuring that safety is not an afterthought but a fundamental principle in pediatric imaging. Collaborative efforts among all stakeholders are key to creating a framework where risks are mitigated effectively.
Technological Innovations and Parental Involvement
Advancements in imaging technology offer a hopeful path toward reducing radiation exposure in pediatric brain CT scans. Innovations such as low-dose CT protocols and automated dose modulation systems can significantly decrease the amount of radiation delivered to sensitive areas like the eye lens while maintaining image quality. Manufacturers and researchers are increasingly focused on developing equipment tailored for pediatric patients, with settings that adjust automatically to a child’s size and needs. Investing in these technologies and ensuring their widespread adoption across medical facilities can transform the landscape of pediatric imaging, making scans safer without sacrificing the precision required for accurate diagnoses.
Parental involvement also plays a pivotal role in advocating for safer imaging practices. Equipping families with clear, accessible information about the risks of radiation and the availability of alternatives empowers them to ask critical questions and participate in decisions about their child’s care. Healthcare providers should prioritize transparent communication, explaining why a CT scan is necessary and discussing potential protective measures. This partnership between medical teams and families can create a shared commitment to minimizing exposure, ensuring that children’s long-term health remains a top priority. By fostering dialogue, the medical community can build trust and encourage a proactive approach to balancing diagnostic needs with safety concerns.
Balancing Diagnostic Needs with Long-Term Health
Navigating the Trade-Offs
The inherent tension between the urgent diagnostic benefits of pediatric brain CT scans and the potential risks of radiation exposure presents a complex challenge for the medical field. On one hand, CT scans provide rapid, detailed insights that are often critical in life-threatening situations such as head injuries or suspected tumors, where delays could have dire consequences. On the other hand, the proximity of the eye lens to the scanned area means that even optimized scans carry some risk of long-term damage, particularly with repeated imaging. Striking a balance requires a nuanced approach that weighs immediate clinical needs against future health implications, ensuring that each scan is justified and conducted with the lowest possible radiation dose to protect young patients.
Collaboration among radiologists, pediatricians, policymakers, and families is essential to navigate these trade-offs effectively. Developing and adhering to evidence-based protocols that prioritize dose reduction without compromising diagnostic accuracy is a starting point. Additionally, fostering open discussions about the necessity of each scan can help avoid overuse, reserving CT imaging for cases where no safer alternative exists. Reflecting on past practices, it became evident that unchecked reliance on CT scans often led to unnecessary exposures, a lesson that shaped today’s push for caution. Moving forward, the focus must be on refining these protocols and ensuring that every decision prioritizes the child’s overall well-being.
Building a Safer Future for Pediatric Imaging
Looking back, the medical community recognized that past approaches to pediatric imaging often underestimated the risks of radiation to structures like the eye lens, prompting a shift toward greater vigilance. The lessons learned drove efforts to implement actionable steps for the future, such as integrating advanced dose-tracking systems to monitor cumulative exposure in real time. Encouraging the development of next-generation imaging tools that further minimize radiation is another priority, alongside expanding access to alternatives like MRI for suitable cases. These innovations, paired with robust training programs for healthcare providers, can pave the way for a safer imaging landscape where risks are systematically reduced.
Reflecting on earlier oversights, it was clear that systemic change required engaging all stakeholders, from clinicians to families, in a shared mission to protect children. Future considerations must include regular updates to safety guidelines based on emerging research, ensuring they remain relevant as technology evolves. Advocacy for funding and policy support to equip hospitals with cutting-edge, low-dose equipment is also crucial. By building on past realizations, the path ahead should focus on creating a culture where safety and diagnostic precision coexist, safeguarding the health of young patients for generations to come.