In the high-stakes world of neurological emergencies, where every passing minute can mean the difference between full recovery and permanent disability, the pressure on clinicians to make rapid, accurate diagnoses is immense. The traditional process of interpreting complex medical images is both an art and a science, heavily reliant on the sharp eye of a trained radiologist who must sift through vast amounts of data to spot subtle, life-threatening abnormalities. However, this human-centric model faces unprecedented strain from rising patient volumes and a persistent shortage of specialized staff. This reality has created a critical need for innovations that can augment clinical expertise, streamline workflows, and enhance the precision of care. Against this backdrop, artificial intelligence is emerging not as a replacement for human skill but as an indispensable partner, a powerful deep clinical AI platform capable of elevating diagnostic performance and delivering measurable benefits across the entire care continuum, from initial detection to long-term monitoring.
Enhancing Diagnostic Precision and Clinical Outcomes
The integration of AI into clinical practice is fundamentally redefining the standards of accuracy and efficiency in diagnosing and managing complex neurological conditions. By leveraging algorithms trained on vast datasets, these intelligent systems can perceive patterns and changes that are often imperceptible to the human eye, providing clinicians with a crucial second opinion that is both objective and consistent. This augmentation of human expertise translates directly into improved patient outcomes, whether by enabling earlier intervention for a growing aneurysm or by accelerating the diagnostic process in the critical window of an acute stroke. The technology acts as a force multiplier, empowering medical professionals to make more informed decisions faster, ultimately saving lives and preserving brain function. These advancements are not merely theoretical; recent scientific findings presented at the 2026 International Stroke Conference underscore the tangible impact of AI across diverse clinical scenarios.
Revolutionizing Aneurysm Monitoring
One of the most compelling demonstrations of AI’s diagnostic superiority lies in the longitudinal monitoring of cerebral aneurysms, where subtle growth over time can signal an increased risk of a catastrophic rupture. A landmark study revealed that an AI-powered platform identified a staggering 46% more instances of clinically significant aneurysm growth when compared to the standard interpretations of neuroradiologists. The AI system successfully detected growth in 27 out of 28 documented cases, a near-perfect record that stands in stark contrast to the 14 cases identified by neuroradiologists alone. This disparity highlights the platform’s exceptional ability to consistently capture minute changes in size and morphology that can easily be missed during routine visual inspection, especially when comparing scans taken months or even years apart. By providing a more reliable and sensitive tool for tracking aneurysm progression, this technology equips clinicians with the critical data needed to make proactive treatment decisions, potentially enabling life-saving interventions before a rupture occurs.
This enhanced capability for aneurysm surveillance signifies a paradigm shift from subjective assessment to data-driven, objective analysis, fundamentally strengthening the safety net for patients under observation. The AI platform serves as a tireless, vigilant adjunct to the clinical team, mitigating the inherent risks of human variability, perceptual error, and diagnostic fatigue. Its consistent performance ensures that no subtle change goes unnoticed, establishing a new gold standard for longitudinal assessment. This level of precision is not just an incremental improvement; it represents a transformation in how rupture risk is evaluated, allowing for a more personalized and evidence-based approach to patient management. For the thousands of individuals living with unruptured aneurysms, this translates into greater peace of mind and the assurance that their condition is being monitored with the highest possible degree of accuracy, ensuring that any dangerous evolution is flagged for immediate clinical attention.
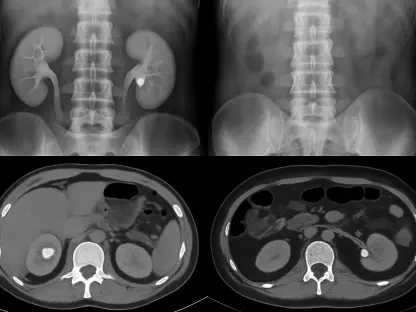
Accelerating Acute Stroke Diagnosis
In the context of acute ischemic stroke, where “time is brain,” the speed and accuracy of diagnosis are paramount to a positive outcome. Research centered on Lumina 3D, an automated 3D reconstruction solution, has proven its immense value in this high-pressure environment. A multi-reader study demonstrated that incorporating this AI tool significantly improved diagnostic accuracy for detecting stroke-related occlusions and stenoses, elevating performance from 76.1% to 85.6%. Beyond this crucial boost in precision, the technology also delivered substantial efficiency gains by reducing the average interpretation time by 34 seconds per case. The benefit was even more pronounced for general radiologists, who saved over a minute on each scan, a critical time saving that can expedite the entire treatment pathway. This dual impact—enhancing accuracy while simultaneously accelerating the workflow—is invaluable in an emergency setting, empowering clinicians to identify critical findings faster and initiate time-sensitive therapies like thrombectomy with greater confidence.
The operational advantages of automated 3D reconstruction extend beyond the reading room, helping to democratize access to high-level expertise across different healthcare settings. In smaller or regional hospitals that may not have 24/7 access to a specialized neuroradiologist, tools like Lumina 3D enable general radiologists to perform with an accuracy that approaches that of their specialist colleagues. This capability is transformative, ensuring a consistent standard of care regardless of a patient’s geographic location. By automating the often time-consuming task of creating detailed 3D vessel reconstructions, the AI frees up clinicians to focus on the most critical aspect of their job: interpreting the images and making a definitive diagnosis. This streamlined process not only accelerates decision-making for individual patients but also enhances the overall throughput of the emergency department, allowing more patients to be evaluated and treated within the critical therapeutic window.
Optimizing Radiology Operations and Economic Viability
Beyond its profound clinical benefits, AI is proving to be a powerful tool for addressing the pressing operational and financial challenges facing modern healthcare systems. The ability of AI-driven automation to optimize workflows and expand capacity offers a direct response to issues like staff shortages and budgetary constraints. By taking over repetitive, time-intensive tasks, these intelligent systems free up highly skilled medical professionals to focus on patient-facing activities and complex decision-making. This enhancement of departmental efficiency is not just about doing more with less; it is about creating a more sustainable and resilient healthcare environment. The economic impact is equally significant, as improved throughput and reduced manual labor translate into a tangible return on investment, making AI a strategic asset for institutions aiming to deliver top-tier care while maintaining financial health.
Streamlining Technologist Workflows
The operational impact of AI automation was powerfully illustrated in a study examining the effect of Lumina 3D on radiology department efficiency, a particularly relevant issue given the nationwide shortage of qualified CT technologists. The implementation of this automated solution led to a dramatic 77.4% reduction in the time technologists spent on complex image reconstructions for each patient. What previously required an average of 31 minutes of hands-on work was condensed to just seven minutes, liberating 24 minutes per scan. When scaled across the department’s workload, this individual time saving amounted to an estimated 81.6 hours of technologist time reclaimed each month. This significant reduction in manual labor not only alleviates the burden on an overstretched workforce, helping to mitigate burnout, but also directly expands the department’s imaging capacity without the need for additional staff, a crucial advantage in a competitive hiring market.
The reclaimed time and enhanced efficiency created a ripple effect, translating directly into substantial financial gains and improved patient access. The 81.6 hours saved per month enabled the facility to perform an additional 108 scans, which in turn generated approximately $43,000 in extra monthly imaging revenue. This demonstrates a clear and compelling economic case for adopting AI-driven automation, showcasing how an investment in technology can yield a significant return by optimizing existing resources. By simultaneously addressing staff workload, expanding imaging capacity, and boosting revenue, the platform provides a holistic solution to some of the most persistent challenges in modern radiology. This synergy of clinical, operational, and financial benefits underscores AI’s role as a transformative force capable of building a more efficient and economically sustainable healthcare ecosystem for the future.
The New Frontier of Intelligent Healthcare
The successful integration of these AI-powered tools ultimately marked a pivotal shift in the landscape of neurological care and radiology. The evidence presented in 2026 clearly established that artificial intelligence was no longer a futuristic concept but a practical and indispensable component of modern medicine. By consistently delivering superior diagnostic accuracy in complex cases like aneurysm monitoring and acute stroke detection, these systems empowered clinicians to intervene with greater confidence and precision. The platforms proved to be more than just analytical engines; they became trusted collaborators that enhanced human expertise, leading to better patient outcomes. This synergy between human intelligence and machine precision became the new standard, fundamentally altering clinical workflows for the better and ensuring that subtle but critical findings were no longer missed.
Furthermore, the operational and economic benefits provided a compelling blueprint for the future of hospital management. The ability of AI to automate time-consuming tasks drastically improved departmental efficiency, which was a critical solution to the pervasive challenge of staff shortages and burnout. This optimization did not just streamline processes; it created tangible value by increasing patient throughput and generating new revenue streams, proving that investments in advanced technology could yield a strong and rapid return. Hospitals and clinics that adopted these solutions found themselves better equipped to handle rising patient loads while delivering a higher quality of care. The advancements showcased throughout the year solidified the role of AI as a cornerstone of a more resilient, efficient, and financially sustainable healthcare system, paving the way for further innovations in patient care.