The journey of pancreatic cancer patient David Allard presents an extraordinary example of how innovative medical interventions can dramatically alter cancer outcomes. Initially diagnosed with stage IV pancreatic cancer, David faced a dire prognosis: less than six months to live. Refusing to accept this outlook, he sought a second opinion at MD Anderson, where a dedicated team of specialists took on his case. Despite the severe challenges posed by a tumor-induced blood vessel obstruction, these experts demonstrated the potential of groundbreaking procedures in reshaping the landscape of cancer treatment, an effort that ultimately extended David’s life.
The Initial Diagnosis and Quest for a Second Opinion
Breaking Through Traditional Prognoses
David’s diagnosis was a turning point that led him to defy the grim six-month survival expectation. By seeking out a second opinion, he demonstrated the importance of exploring all available medical avenues. At MD Anderson, a multidisciplinary team—including Dr. William Ross, Dr. Shubham Pant, and Dr. Eugene Koay—took charge of his treatment. This team approach underscores a growing trend in oncology: the necessity for collaborative care in treating complex cases. Their collective expertise provided David with a tailored treatment plan, which became the foundation of his survival. Such a response to an otherwise terminal diagnosis highlights the significance of not accepting initial prognoses as definitive and the potential benefits of consulting multiple experts.
Addressing Life-Threatening Complications
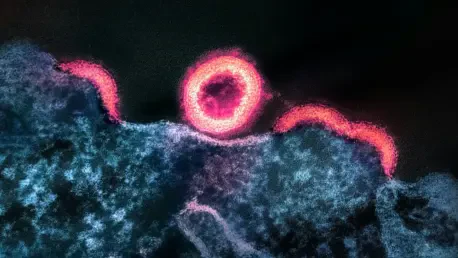
David’s condition was further complicated by a life-threatening issue: internal bleeding caused by portal and splenic vein thrombosis. This was a direct result of the tumor pressing against major blood vessels, creating a barrier to effective cancer treatment. Traditional interventions seemed inadequate, prompting the need for a novel solution. Dr. Peiman Habibollahi, an interventional radiologist at MD Anderson, proposed an innovative approach to overcome this obstacle. Recognizing the complexity and risks involved, his strategy included an image-guided recanalization to reroute the blood flow and the installation of a TIPS to maintain this new pathway. This multifaceted procedure was necessary to stabilize David’s condition, enabling subsequent cancer therapies.
The Role of Innovative Medical Procedures
A Complex Surgical Approach
The complex eight-hour surgery spearheaded by Dr. Habibollahi epitomizes modern medicine’s capability to tackle seemingly insurmountable challenges. The procedure’s success was pivotal in resolving David’s critical bleeding and allowed a recommencement of his cancer treatment. During this intricate surgery, Dr. Habibollahi and his team navigated the complexities inherent in redirecting blood flow and ensuring stability through the TIPS device. The innovative use of image-guided technology played a crucial role in achieving precision, drastically reducing the risks typically associated with such high-stakes surgeries. This highlights a broader potential for advanced surgical techniques to redefine treatment possibilities for patients with complex medical conditions.
Path to Remission Through Persistent Efforts
With his immediate life-threatening issue addressed, David embarked on a rigorous treatment course involving 17 rounds of chemotherapy and three weeks of radiation therapy. This was complemented by ongoing maintenance with the oral chemotherapy agent capecitabine. Collectively, these efforts led to a remarkable outcome: a scan showing no evidence of active disease, with only scar tissue remaining where the tumor once resided. This case illustrates the life-saving impact of innovative and persistent treatment efforts, bolstered by a team’s commitment to patient care. It also hints at a future where such personalized and adaptive interventions become commonplace, allowing more patients to navigate seemingly dire prognoses to successful outcomes.
The Broader Implications of Medical Innovation
Collaboration and Tailored Interventions
David Allard’s experience underscores a fundamental principle in advanced cancer care: the power of collaboration and tailored interventions. His survival story serves as a testament to the effectiveness of a multidisciplinary strategy, drawing on the expertise of various specialists to devise a comprehensive treatment plan. Such collaboration is pivotal in addressing unique challenges faced by patients with complex diagnoses. In this context, MD Anderson emerges as a leader in pushing the boundaries of traditional cancer therapy, offering specialized care not universally accessible. This model of care promises to elevate standards across the medical community, inspiring innovations in both treatment protocols and patient management strategies.
A Paradigm Shift in Cancer Care
David Allard’s battle with pancreatic cancer serves as a remarkable example of how advanced medical interventions can significantly change cancer prognoses. Initially diagnosed with stage IV pancreatic cancer, David was given a grim life expectancy of fewer than six months. Unwilling to accept this fate, he sought out a second opinion at MD Anderson, a leading cancer treatment center, where a dedicated team of specialists took on his case with renewed vigor and determination. Faced with daunting obstacles, including a tumor-caused obstruction of blood vessels, these experts explored cutting-edge procedures that have the power to redefine cancer care. By employing innovative techniques and treatments, they not only extended David’s life beyond the initial expectations but also provided hope for others facing similar challenges. This case underscores the potential of medical advances in transforming dire health situations, illustrating how determination and modern medicine can rewrite patient outcomes in ways once thought impossible.