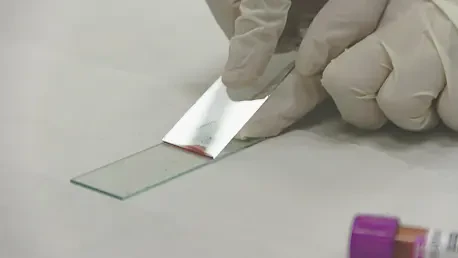
A groundbreaking advancement in dementia diagnostics has emerged as the U.S. Food and Drug Administration (FDA) approved the first blood test for diagnosing Alzheimer’s disease. This new diagnostic tool holds promise by distinguishing Alzheimer’s from other forms of dementia through the detection of specific proteins. Known commercially as the Lumipulse G PUU217/ß-Amyloid 1-42 Plasma Ratio, the test was developed by Fujirebio Diagnostics. It identifies the presence of beta-amyloid and Tau proteins, quintessential in Alzheimer’s pathology, from a simple blood sample. Unlike traditional methods that require expensive PET scans or invasive lumbar punctures, this test offers a less intrusive and more cost-effective alternative, broadening accessibility to a wider patient demographic. However, this test is designed for clinical use by healthcare professionals under specific conditions, primarily focusing on patients over 55 exhibiting symptoms of dementia. To ensure accuracy, prior neuropsychological assessments and brain scans are mandated to rule out other potential causes such as strokes or tumors.
Addressing Current Diagnostic Limitations
PET scans have long been considered a highly reliable method for detecting Alzheimer’s due to their ability to visualize amyloid plaques in the brain. However, their prohibitive cost and limited availability have been significant barriers for many patients. In contrast, cerebrospinal fluid analysis, while informative, demands an invasive lumbar puncture procedure. These conventional approaches, although accurate, pose challenges in terms of accessibility and invasiveness. This newly approved blood test stands as a beacon of hope by addressing these drawbacks, offering sensitivity close to 92%. It provides a specificity of nearly 97% in excluding those without the disease, elevating itself as a formidable contender among diagnostic tools. While PET scans and cerebrospinal analysis remain irreplaceable in certain aspects, the ability to offer easier, less costly testing opens new doors for managing Alzheimer’s disease. This advancement ensures that more patients can be appropriately diagnosed and receive timely interventions, potentially altering the course of their treatment and the progress of their condition.
Despite its potential, this test isn’t without limitations. Less than 20% of the cases might result in indeterminate outcomes, meaning a definitive diagnosis cannot be made solely through this test. Therefore, integrating this test with existing diagnostic methodologies is crucial to avoid any misdiagnosis. The diagnostic precision of this blood test could support a more stratified approach to Alzheimer’s treatment, ensuring patients receive tailored care. Embracing this test in regular clinical practice may provide a middle ground for those unable to access traditional diagnostic modalities, all while maintaining a high standard for diagnostic accuracy. The challenge lies in seamlessly blending it into current medical protocols, ensuring that it complements rather than replaces existing diagnostics. This nuanced use of both new and old methods could prove vital in enhancing the effectiveness of Alzheimer’s diagnostics, ultimately improving patient outcomes.
A Milestone in Alzheimer’s Diagnostics
Historically, blood tests for Alzheimer’s biomarkers were predominantly confined to research settings and lacked commercial approval. The entry of this test into the market signifies not only a technological progression but also a breakthrough in improving diagnostic accuracy and enabling earlier interventions. The role of accurate diagnosis cannot be overstated; it ensures that patients receive the right treatment, avoiding potential side effects from unnecessary medication. Misdiagnosis could lead to detrimental therapeutic courses, emphasizing the essential role of this test in refining treatment paths. For patients and families grappling with memory-related diseases, an accurate diagnosis is the first step to managing the condition effectively.
This regulatory approval also highlights the growing emphasis on early detection and precision medicine in the fight against Alzheimer’s. By integrating new diagnostic solutions with an expanding arsenal of next-generation anti-Alzheimer’s drugs, the medical community is better poised to tackle this prevalent disease. Prospective therapies may be more effective when administered early, offering a glimmer of hope for slowing disease progression. As global populations age, the test’s capability to differentiate Alzheimer’s from other dementias reliably paves the way for better planning and improved quality of life for affected individuals.
Future Implications
A major leap in dementia diagnosis has been achieved with the U.S. Food and Drug Administration (FDA) endorsing the first blood test for Alzheimer’s detection. This innovative tool, named Lumipulse G PUU217/ß-Amyloid 1-42 Plasma Ratio, was developed by Fujirebio Diagnostics. It promises to identify Alzheimer’s from other dementia variations by detecting specific proteins, like beta-amyloid and Tau, crucial to Alzheimer’s disease, via a simple blood sample. Unlike conventional methods reliant on costly PET scans or invasive lumbar punctures, this test provides a more straightforward, budget-friendly alternative, enhancing accessibility for a broader range of patients. Targeting primarily those over 55 showing dementia symptoms, it is designed for clinical use by healthcare professionals under particular conditions. To ensure its precision, prior assessments like neuropsychological tests and brain imaging are imperative to rule out other causes of cognitive impairment, such as strokes or tumors.