In a world where antimicrobial resistance (AMR) stands as one of the most pressing public health crises, the need to scrutinize and optimize the use of antibiotics in healthcare settings has never been more urgent, especially since AMR contributes to ineffective treatments, prolonged illnesses, escalated healthcare costs, and heightened mortality rates. Developing regions such as Latin America bear a disproportionate burden of this challenge, particularly in primary health care (PHC), where the majority of antimicrobial prescriptions are issued, often without adequate oversight or adherence to guidelines. Addressing inappropriate prescribing practices is critical to curbing the spread of resistance, and innovative tools like Electronic Medical Records (EMRs) offer a promising avenue for monitoring and intervention. This article delves into a comprehensive study conducted in São Caetano do Sul (SCS), a Brazilian city with a well-structured health network and a robust EMR system, to evaluate antimicrobial prescription patterns within its public PHC framework. By analyzing data from January to September 2023, the research aims to uncover gaps in prescribing practices for infectious diagnoses and highlight opportunities for targeted interventions. The convergence of public health and data science in this context not only sheds light on current challenges but also paves the way for evidence-based strategies to combat AMR on a local and potentially national scale.
1. Understanding the Context of Antimicrobial Resistance in Brazil
Antimicrobial resistance poses a formidable threat to global health, with Latin America projected to face some of the highest AMR-related mortality rates in the coming decades. In Brazil, the issue is compounded by systemic challenges, including variable access to healthcare and inconsistent application of prescribing guidelines in PHC settings. The overuse and misuse of antibiotics in these environments contribute significantly to the development of resistant pathogens, leading to treatments that fail and infections that persist. São Caetano do Sul, located in São Paulo state, serves as a unique case study due to its relatively advanced health infrastructure, including 12 PHC units that cater to a population of about 165,655 across 15,331 square kilometers. These units provide a range of services, from medical consultations to chronic disease management, all documented through a comprehensive EMR system. This digital infrastructure offers a rare opportunity to analyze real-world data on a city-wide scale, providing insights into how antimicrobials are prescribed and identifying areas where interventions can mitigate resistance risks. The focus on SCS is not just about local impact but also about creating a replicable model for other municipalities facing similar public health challenges.
The significance of leveraging EMRs in this fight against AMR cannot be overstated. These systems allow for the systematic collection and analysis of patient data, enabling health professionals to track prescription trends, monitor adherence to clinical guidelines, and detect patterns of inappropriate use. In SCS, the availability of such data provides a window into the daily operations of PHC, where the bulk of antimicrobial prescriptions occur. The study’s scope, covering medical appointments and drug prescriptions from early to mid-2023, aims to paint a detailed picture of current practices. By focusing on infectious diagnoses, the analysis seeks to understand whether antibiotics are being used appropriately or if there are gaps that need urgent attention. This initial exploration is vital for laying the groundwork for antimicrobial stewardship programs that can reduce unnecessary prescriptions, promote the use of narrow-spectrum drugs, and ultimately slow the progression of resistance within the community. The intersection of public health needs and data-driven insights in this Brazilian city underscores a broader potential for technology to transform healthcare outcomes.
2. Methodology for Data Collection and Analysis
The methodology adopted for this study in SCS relied on a structured approach to extract and analyze data from the city’s public health EMR database. The dataset encompassed a vast array of records from January to September 2023, totaling 3,520,547 entries related to medical appointments, prescribed drugs, and diagnoses across various healthcare facilities. Ethical considerations were paramount, with strict adherence to Brazilian data protection laws ensuring patient confidentiality through anonymization and secure handling of sensitive information. Local ethics committees approved the research, reinforcing compliance with national regulations. The focus was narrowed to PHC units, where 67,023 patients had medical consultations, representing a significant portion of the city’s population. This selection allowed for a targeted examination of antimicrobial use in a setting where most initial prescriptions are made, providing a clear lens through which to view everyday clinical practices.
Data processing followed the Knowledge Discovery in Database (KDD) framework, broken into distinct stages to ensure reliability and relevance. The first step, data collection, involved obtaining raw files in plain text format from EMR exports. The second stage, data refinement, addressed inconsistencies by cleaning records—removing those without patient identifiers and eliminating duplicates—to focus solely on PHC data. Third, data structuring created a relational database with tables for patients, health units, appointments, diagnoses, and drugs, augmented with fields to classify diagnoses as infectious or non-infectious and medications as antimicrobial or non-antimicrobial. Finally, data examination employed statistical and aggregation analyses using tools like SQL, Python, and Plotly, conducted in collaboration with medical experts to ensure clinical accuracy. This meticulous process enabled the categorization of data for detailed analysis, particularly focusing on infectious diagnoses and corresponding prescriptions, setting the stage for meaningful public health insights.
3. Key Findings on Prescription Patterns and Infectious Diagnoses
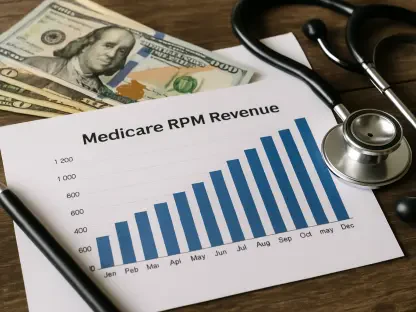
The analysis of 575,616 medical appointment records in SCS revealed critical insights into the health landscape of the city’s PHC system. Of the 67,023 patients who attended consultations, 16,572 were diagnosed with infectious conditions, underscoring the prevalence of such issues in primary care. The most common infectious diagnoses included upper respiratory infections at 37%, gingivitis and periodontal disease at 20%, and urinary tract infections at 9%. These figures highlight the significant burden of respiratory and oral health issues within the community, which often prompt antimicrobial prescriptions. Among the 7,938 antimicrobial prescriptions recorded, amoxicillin led at 23%, followed by azithromycin at 15% and amoxicillin/clavulanate at 13%. This distribution suggests a reliance on certain antibiotics, which may align with the dominant diagnoses but also raises questions about whether these choices are always clinically justified or guideline-compliant.
Further examination through cross-analysis uncovered concerning discrepancies in prescribing practices. Notably, a substantial number of infectious diagnoses did not result in antimicrobial prescriptions—55% of urinary tract infections and 62% of syphilis cases went untreated with antibiotics during the recorded appointments. Conversely, 5,376 consultations involved antimicrobial prescriptions without a documented infectious diagnosis, pointing to potential misuse or documentation errors. An exploratory case study of 40 patient records, split evenly between syphilis and cystitis, provided deeper context. For syphilis, many apparent untreated cases were actually follow-up visits where treatment had already been administered, while cystitis discrepancies included delayed prescriptions and recording errors. Statistically, variations emerged by age and gender, with older patients receiving fewer antibiotics for urinary tract infections (p
4. Challenges and Insights from EMR Data Limitations
While the EMR system in SCS provided a wealth of data for analysis, several technical limitations hindered the depth of insights that could be drawn. A primary challenge was the inability to directly link specific diagnoses to corresponding prescriptions within a single medical appointment. Often, appointments included multiple diagnoses and drugs, but the system lacked a mechanism to indicate which medication was prescribed for which condition. Although most cases with multiple diagnoses featured only one infectious condition, minimizing the impact on overall analysis, this gap still obscured precise correlations. Additionally, inconsistencies in drug naming—sometimes recorded by commercial names rather than chemical compositions—complicated efforts to group and analyze medications systematically. These issues required both computational and manual interventions to ensure data accuracy.
Beyond technical constraints, the empirical nature of diagnoses in PHC settings posed another hurdle. Many infectious conditions, such as respiratory or sexually transmitted infections, were diagnosed without confirmatory tests due to resource limitations, reflecting a broader challenge in Brazil’s healthcare landscape. The lack of integration between laboratory data and EMRs further restricted the ability to validate clinical decisions. These findings underscore the need for improved data capture standards in electronic systems to enhance the reliability of analyses. Addressing such limitations could enable more precise tracking of antimicrobial use, ensuring that health professionals have access to accurate, actionable information. The study’s preliminary results also suggest that while EMRs hold immense potential, their effectiveness depends on structured data entry and seamless integration with other health data sources.
5. Opportunities for Enhancing Antimicrobial Stewardship
The findings from SCS highlight significant opportunities to strengthen antimicrobial stewardship through data-driven approaches. A key observation was the frequent prescription of certain antibiotics like amoxicillin, which, while often appropriate for conditions like respiratory infections, may indicate over-reliance on broad-spectrum options in some cases. Moreover, the absence of antimicrobial treatment for bacterial infections such as cystitis and syphilis in a notable percentage of cases suggests gaps in guideline adherence or documentation practices. Comparing these trends with global studies reveals a consistent pattern of inappropriate prescribing in PHC, often driven by patient expectations or perceived lack of responsibility for AMR development among practitioners. Targeted interventions, informed by real-time data, could address these issues by promoting evidence-based prescribing and reducing unnecessary antibiotic use.
Implementing automated systems to extract and present EMR data logically to health professionals offers a transformative solution. Such systems could flag potential problems, like untreated infections or unjustified prescriptions, enabling policymakers and administrators to design focused interventions. Feedback mechanisms for clinicians, highlighting discrepancies in their prescribing habits, could foster adherence to clinical guidelines. Additionally, standardizing data entry—ensuring diagnoses and prescriptions are clearly linked—would enhance the accuracy of future analyses. Collaboration between data scientists and healthcare providers, as demonstrated in this study, proves essential for translating raw data into actionable public health strategies. By addressing these opportunities, SCS could serve as a model for other regions aiming to combat AMR through technology and interdisciplinary efforts.
6. Future Directions for Public Health Interventions
Reflecting on the analysis conducted in SCS, several critical insights emerged from the examination of EMR data between January and September 2023. The study successfully identified patterns in antimicrobial prescriptions, revealing both strengths and weaknesses in the current PHC system. Despite challenges posed by inconsistent data recording, the richness of information uncovered through cleaning and processing underscored the value of digital health records in public health research. Key areas of concern, such as untreated bacterial infections and undocumented justifications for prescriptions, were brought to light, providing a foundation for targeted improvements. The integration of data science with clinical expertise proved instrumental in navigating these complexities, offering a glimpse into the potential for technology to enhance healthcare delivery.
Looking ahead, actionable steps must be prioritized to build on these findings. Developing automated systems to detect inappropriate antimicrobial prescriptions—considering factors like treatment choice, dosage, and duration—stands as a critical next move. Establishing feedback loops for healthcare providers can address identified gaps, reinforcing evidence-based practices within PHC units. Standardizing data capture in EMRs is essential to ensure that clinical decisions are accurately represented, facilitating more reliable analyses. These efforts, combined with ongoing surveillance and policy adjustments informed by data insights, can strengthen antimicrobial stewardship across Brazil. The lessons learned in SCS highlight the broader need for robust health information systems, offering a pathway to mitigate AMR and improve patient outcomes through informed, technology-supported interventions.