Imagine a scenario where prostate cancer, a leading cause of cancer-related deaths among men globally, can be detected with such precision and speed that lives are saved before the disease even shows symptoms, marking a significant leap in medical technology. A groundbreaking advancement in artificial intelligence (AI) has brought this vision closer to reality through an automated MRI system that’s transforming diagnostics. Powered by cutting-edge deep learning, this tool offers a new level of accuracy in identifying clinically significant prostate cancer, paving the way for earlier interventions and improved patient outcomes. By addressing the shortcomings of traditional screening methods, it promises to redefine how medical professionals approach one of the most pressing health challenges today. This innovation not only enhances diagnostic reliability but also opens doors to equitable healthcare access, making it a pivotal step forward in the fight against cancer.
The Technology Behind the Breakthrough
Unlocking Precision with Deep Learning
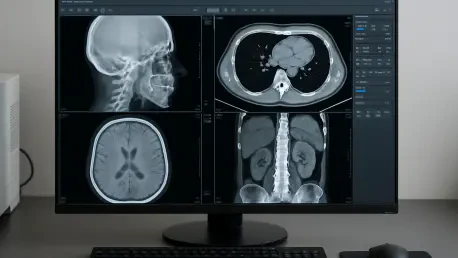
The core of this transformative system lies in its use of advanced deep learning techniques, specifically convolutional neural networks (CNNs), which have been trained on vast datasets of prostate MRI scans. These algorithms excel at recognizing intricate patterns in multiparametric MRI (mpMRI) images, often detecting subtle signs of cancer that might escape even the most experienced radiologists. Unlike traditional methods, where human interpretation can vary widely due to subjective judgment or fatigue, this AI-driven approach delivers consistent results. It analyzes imaging data with a level of detail that matches or surpasses expert performance, marking a significant leap in diagnostic precision. This technology minimizes errors and ensures that potentially life-threatening tumors are identified early, setting a new standard for cancer screening protocols across medical facilities.
Another key aspect of this system is its ability to adapt and learn continuously from new data, refining its accuracy over time. By processing thousands of scans and correlating them with biopsy-confirmed outcomes, the AI builds a robust understanding of what constitutes clinically significant prostate cancer. This ongoing improvement means the system isn’t static; it evolves to handle diverse imaging protocols and patient demographics. Such adaptability is crucial in a field where technology and medical needs are constantly shifting. The reduction in diagnostic variability offers a reliable foundation for doctors to make informed decisions, ultimately benefiting patients who rely on timely and accurate detection for effective treatment planning.
Tackling Overdiagnosis in Screening
One of the most pressing issues in prostate cancer screening has been overdiagnosis, where benign or slow-growing conditions are mistaken for aggressive tumors, leading to unnecessary procedures. This AI system addresses that challenge head-on by distinguishing between cancers that require immediate intervention and those that pose little threat. Its high sensitivity and specificity, validated across varied patient groups, ensure that only clinically significant cases are flagged for further action. This targeted approach reduces the emotional and physical burden on patients who might otherwise undergo invasive biopsies or treatments without cause, preserving their quality of life.
Beyond just improving patient experience, this focus on meaningful detection has broader implications for healthcare systems. By cutting down on unwarranted interventions, the system helps allocate medical resources more efficiently, directing attention to those in genuine need. The precision in identifying significant tumors also builds trust in diagnostic processes, as patients and clinicians alike can rely on results that prioritize health outcomes over excessive caution. This balance between caution and necessity represents a critical advancement, reshaping how screening programs are designed and implemented on a global scale.
Clinical Integration and Practical Benefits
Enhancing Workflow Efficiency
Integrating this AI-powered MRI system into clinical environments has proven to be a seamless process, largely due to its design for real-world application. It processes scans at a remarkable speed, alleviating the bottlenecks often experienced in busy radiology departments where time is of the essence. This rapid turnaround allows hospitals to handle higher volumes of patients without compromising on diagnostic quality. Additionally, the system generates intuitive outputs such as heatmaps and lesion segmentations on MRI images, providing visual aids that simplify complex data. These tools empower radiologists to make quicker, more confident decisions while facilitating clearer communication during treatment planning and patient consultations.
The practical benefits extend to multidisciplinary collaboration within healthcare teams. The visual outputs serve as a common reference point, enabling oncologists, urologists, and radiologists to align on the best course of action for each patient. This streamlined approach not only saves time but also enhances the overall quality of care by ensuring all stakeholders have access to the same actionable insights. Furthermore, by reducing the manual workload on radiologists, the system helps mitigate burnout—a growing concern in the medical field. The result is a more efficient clinical workflow that prioritizes both patient needs and staff well-being, setting a precedent for how technology can support modern medicine.
Prioritizing Ethics and Privacy
A standout feature of this system is its commitment to ethical standards, particularly in safeguarding patient data. Utilizing a federated learning framework, it allows for continuous model improvement without centralizing sensitive information, thus protecting privacy. This method ensures that hospitals and research institutions can contribute to the AI’s development while adhering to strict confidentiality protocols. Such an approach is vital in an era where data breaches pose significant risks, reinforcing trust in technology-driven healthcare solutions. It demonstrates that innovation and ethics can coexist, addressing public concerns about AI in medicine.
Equally important is the system’s role as an assistive tool rather than a replacement for human expertise. Designed to support radiologists, it enhances their capabilities without undermining clinical oversight. This balance ensures that critical decisions remain in the hands of trained professionals, with AI providing valuable insights to inform those choices. The emphasis on transparency—through clear, interpretable outputs—further ensures accountability in its application. By maintaining human judgment at the forefront, the system aligns with medical ethics, fostering a collaborative environment where technology and expertise work in tandem to improve patient care.
Broader Impact on Public Health
Addressing Disparities in Care
One of the most promising aspects of this AI-powered MRI system is its potential to bridge gaps in prostate cancer care, particularly in regions with limited access to specialized radiologists. In many underserved areas, the scarcity of expertise often delays diagnosis, leading to worse outcomes for patients. This technology offers a solution by delivering high-quality diagnostic support regardless of local resources, ensuring that even remote or economically disadvantaged communities can benefit from advanced screening. Such democratization of care could significantly reduce disparities, bringing equity to a field where geography and income have long dictated health outcomes.
The impact on global health equity cannot be overstated. By reducing reliance on a small pool of highly trained specialists, the system enables broader implementation of effective screening programs in low-resource settings. This scalability means that countries with strained healthcare systems can still prioritize early detection, potentially lowering mortality rates. Additionally, partnerships with international health organizations could further amplify its reach, ensuring that the benefits of this innovation are felt worldwide. The focus on accessibility underscores a vital shift toward inclusive healthcare, where technology serves as a leveling force for all populations.
Transforming Screening Programs
From a public health perspective, the affordability and scalability of this system position it as a powerful tool for transforming prostate cancer screening initiatives. By minimizing unnecessary procedures through precise detection, it offers substantial cost savings for healthcare systems, a factor that has garnered attention from policymakers and insurers. These savings can be redirected to expand screening coverage or fund other critical health programs, amplifying the overall impact on community well-being. The economic benefits align with the clinical advantages, creating a compelling case for widespread adoption across diverse regions.
Moreover, the system’s ability to improve early detection rates holds the potential to save countless lives on a global scale. Early identification of clinically significant cancers often translates to more treatable conditions, reducing the burden of advanced-stage disease on both patients and healthcare infrastructures. As governments and health organizations recognize these advantages, support for integrating AI-driven diagnostics into national health strategies continues to grow. This momentum suggests a future where advanced technology becomes a cornerstone of public health efforts, fundamentally reshaping how societies approach cancer prevention and management.
Future Potential and Challenges
Pioneering AI Applications in Oncology
Looking ahead, this automated MRI system serves as a pioneering model for AI applications beyond prostate cancer, with implications for other oncological fields such as breast, brain, and liver cancer detection. The methodologies developed—particularly the use of deep learning to interpret complex imaging data—provide a blueprint that can be adapted to various diseases. This cross-disciplinary potential highlights the versatility of AI in medical imaging, where lessons learned from one area can accelerate progress in others. The success of this tool underscores the growing role of technology in enhancing diagnostic capabilities across the spectrum of healthcare challenges.
The vision for the future extends even further, with researchers exploring ways to integrate MRI data with multi-omics information, including genetic, proteomic, and metabolomic markers. Such a comprehensive approach could usher in an era of truly personalized medicine, where diagnostics not only identify cancer but also predict how it might respond to specific treatments. This level of customization would allow for tailored therapeutic strategies, optimizing outcomes for individual patients. The ambition to create a holistic diagnostic platform reflects the transformative power of AI, promising a future where disease management is as unique as the patients themselves.
Overcoming Hurdles for Inclusivity
Despite its remarkable achievements, the system faces challenges that must be addressed to ensure its effectiveness across all contexts. A primary concern is the need for high-quality MRI equipment, which may not be readily available in all regions. Without consistent imaging standards, the AI’s performance could be compromised, limiting its benefits in resource-constrained environments. Efforts are underway to develop solutions that accommodate varying equipment capabilities, ensuring that the technology remains viable even in less-equipped facilities. This focus on adaptability is crucial for maintaining the system’s promise of global accessibility.
Another critical issue is the diversity of data used to train the AI, as underrepresentation of rare cancer subtypes or specific demographics could introduce bias. To counter this, ongoing validation studies and inclusive recruitment strategies are being prioritized to build a more comprehensive dataset. Such measures aim to refine the system’s accuracy and fairness, ensuring it serves a wide range of patients effectively. The commitment to continuous improvement and transparency in addressing these limitations reflects a dedication to creating a tool that is not only innovative but also equitable, paving the way for sustained impact in medical diagnostics.