While the healthcare industry debates electronic health record interoperability, consumer tech is redefining user expectations. The annual Consumer Electronics Show (CES) has long served as a barometer for technological momentum, and this year’s showcase delivered a clear verdict: AI is the new operating system for daily life. For healthcare leaders, the product unveilings offered a direct look at the emerging landscape they must navigate.
The shift from siloed AI applications to deeply embedded, ecosystem-wide intelligence signals a fundamental change. It’s a change in how products are designed, services are delivered, and how users interact with the digital world. Patients, accustomed to seamless and predictive consumer experiences, will soon demand the same from their healthcare providers. Ignoring this shift is not an option.
Continue reading to discover how consumer-grade AI is quietly reshaping care delivery, redefining patient expectations, and forcing healthcare leaders to rethink what “digital transformation” really means.
From Feature to Foundation
The most significant narrative to emerge from the consumer tech world is the transition of AI from a discrete function to a foundational layer. This change is powered by monumental leaps in the underlying infrastructure that will soon filter into the medical field. For example, chip advancements designed to manage trillion-parameter models are not just for consumer devices, they lay the groundwork for making large-scale medical AI economically viable.
The goal is to dramatically reduce the cost of AI inference, enabling real-time analysis of complex medical imaging or genomic data sets at scale. This foundational power is what will enable the next generation of sophisticated, user-facing health assistants.
Imagine a personal health agent that operates as a “fused knowledge base” across a patient’s devices. It would integrate data from wearables, EHRs, pharmacy records, and lifestyle apps to create a living digital model that anticipates needs and performs complex tasks. This moves beyond simple appointment reminders toward deeply personalized, context-aware agents that are perpetually learning and providing proactive health guidance.
Ambient Intelligence in the Clinical Setting
This embedded intelligence is finding its most powerful expression in the physical world, particularly within clinical environments. The aim is to create “smart” spaces that reduce administrative burdens and enhance patient safety. Devices are moving beyond simple programmed tasks to exhibit adaptive, intelligent behavior that supports clinicians, rather than adding to their workload.
In the hospital, this trend translates to ambient listening technologies that can securely capture doctor‑patient conversations. These systems use natural language processing to auto‑populate EHRs, draft clinical notes, and queue up orders for prescriptions or labs. The impact on physician burnout is significant. In fact, studies of ambient AI scribe platforms have shown reductions in documentation time of roughly 22–29%, meaning clinicians spend substantially less time on admin work and more time on patient care, a key factor linked to reduced burnout and improved workflow efficiency.
This extends to the patient room itself. AI-powered monitoring systems can use optical sensors to track a patient’s heart rate, respiratory rate, and movement patterns without physical contact. These systems can detect subtle signs of deterioration hours before a human observer might, or identify when a patient is at high risk of a fall. It’s a shift from reactive care to a proactive, data-driven model of patient safety.
Revolutionizing the Patient Experience
The pervasive integration of AI is also set to fundamentally reshape the patient journey, driving a more personalized and engaging standard of care. The one-size-fits-all approach to patient engagement is becoming obsolete. The future of healthcare delivery will be intelligently optimized for individual patient needs and preferences.
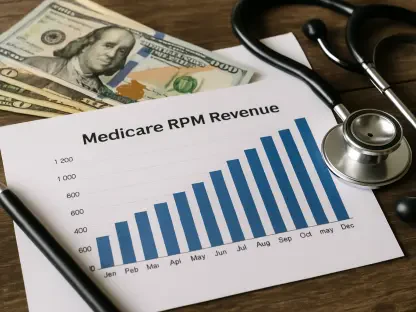
Consider the management of chronic diseases like diabetes or hypertension. A new generation of remote patient monitoring (RPM) platforms uses AI to move beyond simple data collection. They analyze trends, predict potential adverse events, and deliver personalized interventions directly to the patient.
For example, one health system’s pilot program equipped diabetic patients with an AI-powered RPM platform. The system analyzed real-time glucose data, meal logs, and activity levels to provide personalized coaching and alerts. This intervention reduced hospital readmissions for this high-risk cohort by 15% and improved key glycemic control metrics by 20% within the first year.
This hyper‑personalization extends to communication. Conversational AI can now manage post‑discharge follow‑up, answer common patient questions, and triage concerns to the appropriate care team member. This ensures patients feel supported after leaving the hospital and helps clinical teams manage their caseloads more effectively. The global healthcare chatbot market, a key enabler of these capabilities, was valued at about $1.2 million in 2024 and is projected to continue growing strongly in the coming years, reflecting rapid adoption of AI‑driven patient engagement tools across care settings.
Navigating the Regulatory and Ethical Minefield
While the opportunities are immense, HealthTech leaders must approach AI implementation with a clear understanding of the unique challenges in healthcare. Unlike the consumer world, the stakes are infinitely higher. A flawed recommendation from a shopping algorithm is an inconvenience; a flawed diagnostic recommendation can have life-or-death consequences.
Data privacy and security are paramount. All AI systems must be designed from the ground up to be compliant with HIPAA and other stringent data protection regulations. The industry is also grappling with the “black box” problem, where the reasoning behind an AI model’s conclusion is not always transparent. For AI to be trusted in clinical decision support, its outputs must be explainable and auditable.
For example, one health system’s pilot program equipped diabetic patients with an AI-powered RPM platform. The system analyzed real-time glucose data, meal logs, and activity levels to provide personalized coaching and alerts. In practice, studies of remote monitoring programs for diabetes have shown reductions in hospital readmissions of up to about 22% and meaningful improvements in glycemic control, highlighting how connected, data-driven interventions can improve outcomes for high-risk patients.
Conclusion
The signal from CES is about a reset in how intelligence shows up everywhere, quietly raising the bar for trust, responsiveness, and relevance. Systems built for yesterday’s constraints will feel increasingly out of sync with how people live, decide, and expect support.
The organizations that win won’t be the ones with the flashiest pilots, but the ones that treat AI as a long-term design philosophy rather than a bolt-on experiment. This is a moment for intentional leadership: setting guardrails early, choosing leverage points wisely, and building confidence through execution.
Get that right, and healthcare doesn’t just keep pace with consumer expectations, it reclaims its role as the most human application of technology there is.