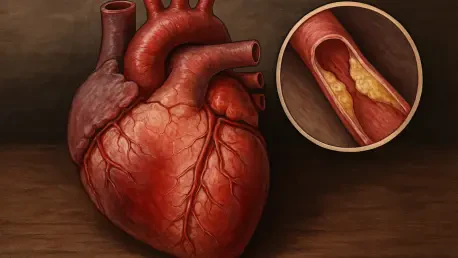
In the Deep South, the prevalence of heart disease remains a pressing concern that demands urgent attention, particularly in Mississippi, where it stands as a leading cause of mortality. Researchers at the University of Mississippi have undertaken a comprehensive investigation to unpack the complex web of social and structural elements influencing heart health across five Southern states. Led by Ruaa Al Juboori and Andrew Yockey, this study seeks to discern the interplay between these elements and their cumulative impact on cardiovascular diseases, aiming to uncover strategies that can effectively mitigate heart-related risks. The scope of this research spans over 400 counties, capturing a wide spectrum of socioeconomic conditions and health disparities, with a primary focus on coronary heart disease (CHD). Central to their findings is the understanding that healthcare accessibility, geographical disparities, socioeconomic challenges, and innovative initiatives play pivotal roles in shaping the heart health of these communities.
Healthcare Accessibility and Provider Availability
One of the core themes identified by the research is the critical role that healthcare provider availability, particularly primary care physicians, plays in mitigating heart disease risks. In areas where the number of practicing primary care doctors is limited, there is a noticeable increase in cardiovascular complications. The findings reveal that even modest increases in primary care availability can significantly enhance coronary health outcomes. Hence, it is essential to prioritize investment in rural healthcare infrastructure—initiatives such as loan forgiveness programs for medical practitioners and rural residency incentives are crucial. These solutions not only enhance workforce capacity but also serve as vital measures to decrease CHD rates and reduce mortality in the long term. The necessity of bolstering the number of healthcare providers cannot be overemphasized, as it forms the backbone of any strategy aimed at curbing the heart disease epidemic.
Geographical disparities in the availability of healthcare services further exacerbate the challenges faced by many regions. The Mississippi Delta and western Alabama, for example, struggle with chronic shortages of healthcare professionals alongside deeply entrenched poverty. These areas serve as prime examples where residents often grapple with insufficient access to medical care, a factor that significantly contributes to the elevated rates of heart disease-related deaths witnessed there. Addressing this disparity necessitates a comprehensive approach, one that not only aims to attract medical professionals through incentives but also focuses on building sustainable, community-engaged health systems that can operate effectively within these socioeconomically marginalized settings.
Geographical and Socioeconomic Disparities
This investigation into heart health also sheds light on the pronounced geographical health disparities within the Southern United States, particularly highlighting areas such as the Mississippi Delta. Here, socioeconomic adversities and a sparse healthcare workforce combine to exacerbate cardiovascular risks. The study emphasizes that understanding these intricate dynamics plays an indispensable role in formulating any effective health intervention strategy. The disparities are further intensified by factors such as poverty, which limits individuals’ access to necessary health services and healthy lifestyle choices. To address these challenges, a reinforced infrastructure and strategically crafted policies are crucial, helping to ensure that vulnerable populations receive adequate medical attention and preventive care.
In addition to economic shortcomings, these regions are often plagued by a lack of educational resources and opportunities, which significantly impact health literacy and the ability of individuals to engage in health-promoting behaviors. Without sufficient education and health literacy, efforts to prevent and manage heart disease are notably undermined. Bridging the knowledge gap is essential and requires implementing comprehensive educational programs that are culturally sensitive and linguistically accessible. These initiatives can empower communities to make informed health decisions, thus reducing the overall incidence of heart-related conditions. Ultimately, addressing the socioeconomic and educational disparities paves the way for more equitable health outcomes across the region.
Innovative Initiatives and Positive Outcomes
The study also explores regions that, despite facing structural challenges, report unexpectedly positive cardiovascular outcomes, such as Washington County in Alabama and Treutlen County in Georgia. These areas benefit from progressive state-supported health initiatives, showcasing that strategic, targeted efforts can yield substantial health improvements even under resource-constrained circumstances. Initiatives like the Georgia Rural Health Innovation Center have expanded telehealth services and enlisted community health workers to deliver education and support. Such programs demonstrate that when communities are equipped with the necessary tools and support, favorable health outcomes can be achieved regardless of initial constraints.
The success of these interventions underscores the importance of adopting adaptive and community-focused health solutions, where local insights and strengths are leveraged to tailor strategies suited to specific regional needs. Innovations do not occur in isolation but rather within the context of broader systemic support that actively engages with community members and integrates their feedback into the planning and delivery of health services. Moreover, harnessing technology, coupled with grassroots community involvement, enables the dismantling of health barriers and fosters a collaborative environment conducive to sustaining health improvements over the long term.
Social and Lifestyle Determinants
The influence of social and lifestyle factors on cardiovascular risks is diverse and varies greatly from county to county. Elements such as income levels and demographic factors like aging populations and access to healthcare and technology starkly define the health challenges and strengths within these regions. Counties with higher income levels and greater technological access have shown evidence of stronger health outcomes, accentuating the role of socioeconomic status in determining community health profiles. Recognizing these determinants is vital in formulating interventions that are not only effective but also sustainable over time.
Conversely, areas facing economic constraints and a lack of access to technology encounter multiple barriers that impede the potential for health improvement. These challenges are compounded by lifestyle factors, including dietary habits, physical inactivity, and tobacco use, which prevail due to a combination of cultural, educational, and environmental influences. Addressing these obstacles requires a multifaceted approach that combines education, community engagement, and policy advancements aimed at promoting healthier lifestyles. By fostering environments that support improved lifestyle choices, significant strides can be made in reducing cardiovascular risks and enhancing the overall well-being of these communities.
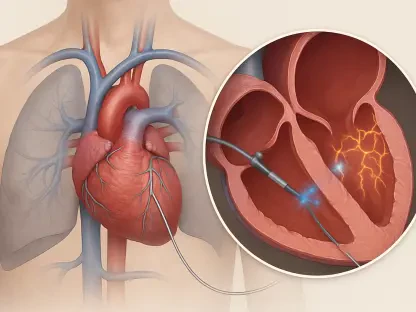
Role of Telehealth and Technology
The study accentuates telehealth as a promising avenue to ameliorate healthcare disparities in rural areas where provider density is low. However, it is evident that technology on its own is insufficient to bridge the healthcare gap effectively. A hybrid model that blends digital tools with robust local healthcare stress the community-based support is deemed necessary to harness telehealth’s full potential. Issues such as broadband access and digital literacy must be addressed to ensure equitable technology use across diverse communities. Enhancing telehealth infrastructure could significantly increase accessibility, making healthcare more inclusive for marginalized populations and extending the reach of medical services far beyond traditional settings.
Examining health models from more affluent regions, like Denver, Colorado, offers valuable insights into successful health strategies. Their low heart disease rates can be attributed to a synergy of well-utilized resources, extensive physical activities, and a priori emphasis on preventive care. Learning from these models allows for the adaptation of effective health strategies that can be tailored to the cultural and socioeconomic contexts of the Southern states. Such comparisons provide a blueprint for implementing robust and comprehensive telehealth and healthcare strategies that focus on local needs and capabilities, fostering advancements in healthcare equity.
Future Directions and Holistic Approach
Heart disease is a major issue in the Deep South, demanding urgent action, especially in Mississippi, where it remains a top cause of death. Researchers from the University of Mississippi are delving into the intricate social and structural factors affecting heart health in five Southern states. Spearheaded by Ruaa Al Juboori and Andrew Yockey, this study aims to understand how these factors interplay to affect cardiovascular health and to identify ways to reduce heart disease risks. The research spans over 400 counties, addressing a wide range of socioeconomic conditions and health inequalities. The main focus is on coronary heart disease (CHD). Key findings emphasize that access to healthcare, geographical differences, socioeconomic hurdles, and new initiatives significantly influence heart health in these areas. This comprehensive approach not only highlights the root causes but also guides the development of targeted interventions to enhance cardiovascular health outcomes in these at-risk communities.