The agonizing wait for a critical medical diagnosis, a period fraught with anxiety for patients and their families, is increasingly being prolonged by a severe global shortage of the specialists needed to interpret life-saving medical scans. This bottleneck in the diagnostic pipeline not only delays vital treatments but also places immense pressure on overburdened healthcare systems. In response to this crisis, Scotland has emerged as an unlikely global epicenter of innovation, pioneering the integration of artificial intelligence into radiology. This technological revolution is not about replacing the invaluable expertise of radiologists but about augmenting their capabilities, creating a powerful human-machine partnership that streamlines workflows, accelerates diagnoses, and is fundamentally reshaping the future of medical imaging for the better.
Redefining the Diagnostic Pipeline with Intelligent Automation
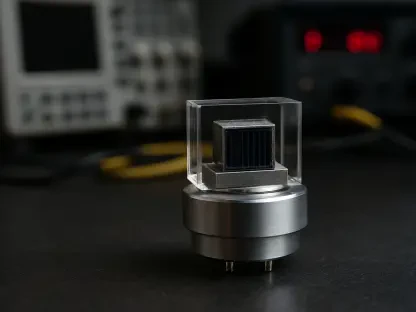
The traditional journey from a patient undergoing a scan to receiving a final diagnostic report can be a disjointed and lengthy process, sometimes taking weeks to complete. Artificial intelligence is now being strategically deployed to re-engineer this entire timeline, with the potential to condense it into a matter of hours. This transformation begins at the very start of the process: image acquisition. Innovators like Canon Medical Research Europe are at the forefront, developing AI-driven technology such as “Automated Landmark Detection.” This system utilizes a low-resolution preliminary scan to allow an algorithm to intelligently pinpoint areas of interest that necessitate a more detailed, high-resolution inspection. By automating the scan planning phase, a task historically performed manually by a radiographer, significant cumulative time savings are achieved over the course of a day’s work. Furthermore, this technology helps to automate radiation exposure levels, optimizing the delicate balance between patient safety and image clarity. By using advanced reconstruction algorithms, AI can enhance the quality of images captured with lower radiation doses, providing a dual benefit of efficiency and improved patient care.
Once a medical image is acquired, AI transitions into its role as a crucial support and triage tool for radiologists, helping them navigate the ever-increasing volume of scans. Companies such as Annalise are developing sophisticated systems that automatically analyze images to flag potential areas of concern, acting as a highly efficient first line of review. This capability is particularly transformative in the triage process. AI algorithms can rapidly sift through large datasets of scans, prioritizing those that exhibit signs of urgent or life-threatening conditions for immediate attention from a human specialist. Concurrently, these systems excel at identifying and filtering out scans that show no significant abnormalities. This “clearing of negatives” represents a profound efficiency gain, as it removes a substantial portion of the routine workload from the radiologist’s queue. This ensures that the limited and highly valuable time of clinical experts is concentrated on the most complex and critical cases, directly accelerating the diagnostic pathway for patients who need it most.
From Theoretical Promise to Measurable Clinical Impact
The integration of these AI tools is already delivering tangible, life-altering results in clinical settings far beyond Scotland’s borders. In one striking example from a German hospital, an AI detection algorithm identified the subtle signs of a large-vessel occlusion—a major blockage in a brain artery causing a severe stroke—within minutes of the patient’s scan. This immediate alert enabled the medical team to escalate the patient to a time-sensitive thrombectomy procedure much more rapidly than would have been possible through traditional review processes. The swift intervention, facilitated by AI, was a critical factor in the patient’s full clinical recovery, powerfully demonstrating the technology’s capacity to save lives in time-critical medical emergencies. This success story moves AI from an abstract concept to a proven clinical asset, capable of making a decisive difference in acute care scenarios where every second counts.
The impact of AI extends beyond acute emergencies to deliver system-wide efficiencies that benefit entire patient populations. At a university hospital in the United Kingdom, the implementation of an AI system in its busy emergency and fracture clinics allowed for the immediate clearance of scans with negative findings. This straightforward application effectively automated the review of thousands of routine cases, saving an estimated 400 hours of patient waiting time and substantially alleviating the immense pressure on clinical staff. On an even larger scale, a hospital system in Norway deployed an AI-powered triage system that assisted radiologists in rapidly clearing over 8,500 negative chest X-rays from their worklists. This single, focused intervention resulted in a cumulative reduction in patient wait times equivalent to 250 days. These examples showcase how AI is not just a tool for individual diagnoses but a powerful platform for optimizing healthcare operations, improving patient throughput, and creating a more resilient and responsive health service.
The Foundation of Success a Uniquely Collaborative Ecosystem
Scotland’s rapid emergence as a leader in medical imaging AI is not a coincidence but the product of a uniquely fertile and collaborative innovation ecosystem. The progress is fundamentally driven by a “triple helix” model that fosters deep, synergistic partnerships between pioneering private industry leaders, world-class academic and research institutions like Glasgow’s Imaging Centre of Excellence, and the extensive clinical expertise within the publicly funded National Health Service (NHS). This integrated approach creates a virtuous cycle: industry develops cutting-edge technology, academia provides rigorous research and validation, and the NHS offers the real-world clinical setting for testing and deployment. This close-knit collaboration accelerates the entire innovation pipeline, allowing promising concepts to be developed, refined, and implemented into patient care pathways far more quickly than in more fragmented environments. This culture of partnership is widely cited as Scotland’s key strategic advantage in the global health-tech landscape.
This dynamic ecosystem is built upon a solid foundation of significant structural and data-driven advantages. A key element is the NHS in Scotland’s use of the Community Health Index (CHI) number, a unique patient identifier that allows for the longitudinal linking of an individual’s health data across different services over their entire lifetime. This creates comprehensive, anonymized datasets that are an invaluable resource for training, testing, and validating the accuracy and efficacy of AI algorithms. Furthermore, this infrastructure is complemented by a robust pipeline of world-class talent in AI and data science graduating from Scottish universities, as well as active government support for digital health initiatives. The proven track record of successful commercial partnerships further strengthens this environment, creating a self-reinforcing cycle of investment, innovation, and clinical implementation that continues to attract talent and capital, solidifying Scotland’s position at the vanguard of medical technology.
A New Blueprint for the Future of Medical Imaging
The initiatives in Scotland conclusively demonstrated that the most effective application of artificial intelligence was not to replace the radiologist but to augment their expertise and fundamentally optimize the diagnostic workflow. By successfully automating routine tasks, intelligently prioritizing urgent cases, and streamlining the end-to-end process, the technologies developed and deployed delivered measurable and profound improvements. These advancements resulted in accelerated diagnoses, significantly reduced patient wait times, and enhanced operational efficiency across the healthcare system. The success of this endeavor was intrinsically linked to Scotland’s unique and robust ecosystem, which masterfully integrated industry innovation, academic rigor, and daily clinical practice. This collaborative model ultimately established a powerful blueprint for how nations around the world could harness AI to create a more sustainable, efficient, and patient-centric future for medical imaging.