The fundamental shift within the American healthcare system towards a value-based care model has created an urgent need for evidence that extends beyond the pristine conditions of randomized clinical trials. For decades, the industry has wrestled with a central challenge: how to deliver the best possible patient outcomes at a sustainable cost when the primary evidence for a treatment’s worth comes from studies involving highly selective patient groups. These traditional trials, while the gold standard for proving efficacy, often fail to reflect the complexities of real-world patient populations, who present with multiple comorbidities, varying levels of treatment adherence, and diverse demographic backgrounds. This discrepancy creates a significant knowledge gap for payers, providers, and life science organizations. Real-World Evidence (RWE) has emerged as the critical bridge, offering a more comprehensive and accurate understanding of how medical interventions perform in the context of everyday clinical practice, thereby becoming an indispensable tool for navigating modern healthcare.
The Expanding Universe of Healthcare Data
Real-World Evidence is meticulously compiled from a vast and growing ecosystem of data sources that chronicle the complete patient experience far beyond the confines of a research study. This rich tapestry of information includes detailed clinical notes from electronic health records (EHRs), financial insights from claims and billing data, and increasingly, patient-generated data from wearable devices and mobile health applications. The continuous proliferation of digital health technologies is accelerating the collection of real-time data at an unprecedented scale, transforming RWE into a dynamic and powerful resource. This evolution has not gone unnoticed by regulatory authorities. Influential bodies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) are now actively encouraging the integration of RWE into their decision-making processes, signaling a major shift in how the safety and effectiveness of treatments are evaluated and monitored throughout their lifecycle.
The escalating importance of RWE is now a widely accepted industry consensus, cementing its position as a cornerstone of modern healthcare strategy rather than a supplementary concept. A recent survey highlighted RWE as one of the most impactful trends currently shaping the industry, a sentiment echoed by stakeholders across the spectrum. Its true value lies in its ability to generate genuinely representative and longitudinal data that reflects the heterogeneity of actual patient populations. Unlike clinical trials, which are time-limited and operate under idealized protocols, RWE captures the long-term impact of therapies on individuals with complex health profiles. This provides a more realistic assessment of a treatment’s benefit-risk profile over time, enabling a deeper understanding of its performance in groups often underrepresented in trials, such as the elderly or those with multiple chronic conditions, thus generating insights that are essential for true value-based care.
Navigating the Complexities of Data Integration
Despite its enormous potential, the effective utilization of Real-World Evidence is frequently impeded by significant infrastructural and technical barriers inherent in the healthcare industry. The data ecosystem is notoriously fragmented, with vital patient information often locked away in disparate, siloed systems that lack interoperability. This fragmentation makes it extraordinarily difficult to create a holistic view of a patient’s health journey. Compounding this issue is the lack of standardized data collection methods across different healthcare organizations, which leads to inconsistencies that complicate aggregation and analysis. Furthermore, a substantial portion of clinically rich information is captured in unstructured formats, such as the narrative text within physician notes or diagnostic images embedded in EHRs. This lack of integration and standardization presents a formidable challenge to data sharing and the advanced analytics required to convert raw data into actionable intelligence.
Overcoming these deeply entrenched data hurdles requires the deployment of sophisticated technologies capable of navigating this complex landscape. Artificial intelligence (AI) and machine learning (ML) have become essential tools for this purpose, offering the computational power needed to process vast and varied datasets at scale. These advanced analytical engines can sift through unstructured information, using natural language processing to extract meaningful clinical concepts from physician notes and other text-based sources. They can also harmonize and standardize data from different systems, creating cohesive, high-integrity datasets suitable for rigorous analysis. By automating these once-manual and time-consuming processes, AI and ML are unlocking the full potential of RWE, transforming a chaotic collection of information into a structured and powerful asset that can support clinical research, regulatory submissions, and value-based care initiatives.
Transforming Decision-Making for Payers and Providers
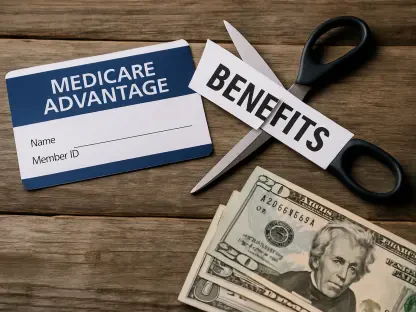
For payers operating within a value-based reimbursement environment, Real-World Evidence has become a particularly transformative asset. In a system where payments are increasingly tied to patient outcomes, payers require robust evidence that a therapy is not just efficacious in a trial setting but also effective and cost-efficient for the diverse populations they insure. RWE delivers this crucial proof by demonstrating how treatments perform under routine clinical care, taking into account critical variables like differing patient demographics, the presence of multiple comorbidities, and real-world patterns of medication adherence. This detailed insight closes a significant knowledge gap left by traditional clinical trials, allowing payers to understand which specific patient subgroups benefit most from a therapy, under what conditions those benefits are realized, and how consistently positive outcomes are achieved across their member base, leading to more precise coverage decisions.
Beyond confirming clinical effectiveness, RWE facilitates a more nuanced and accurate cost-benefit analysis, empowering payers to optimize resource allocation. By linking specific treatment choices to downstream health outcomes—such as hospital readmissions, emergency department visits, or the utilization of other healthcare services—it becomes possible to directly compare the real-world cost-effectiveness of different therapeutic pathways. This data-driven approach helps identify and promote clinical practices that consistently deliver superior results, thereby reducing costly care variability. It also enables enhanced safety monitoring over extended periods, allowing for the early detection of adverse events that may not surface during the limited timeframe of a clinical trial. Armed with this comprehensive evidence, payers are better positioned to negotiate value-based contracts with manufacturers and refine their formulary designs to prioritize interventions that offer demonstrable, real-world value.
A New Era of Collaborative Healthcare
The influence of Real-World Evidence extends across the entire healthcare ecosystem, fostering a more collaborative and informed environment for all stakeholders. Biopharmaceutical researchers, for instance, leverage these robust datasets to gain deep clinical insights that inform and improve the design, planning, and recruitment for future clinical trials, making them more efficient and representative. Government agencies rely on RWE for comprehensive post-market surveillance, enabling them to continuously monitor the long-term safety and effectiveness of approved treatments and identify unmet medical needs within the population. Simultaneously, commercial biopharma teams utilize RWE to build a compelling value proposition that goes beyond the initial trial data, demonstrating a therapy’s tangible benefits and economic advantages to payers and health systems, which is crucial for securing market access and achieving favorable formulary placement in an increasingly competitive landscape.
The integration of these powerful data streams into daily practice ultimately depended on establishing networks that seamlessly connected providers, payers, and life science organizations. The operationalization of RWE was achieved through platforms that facilitated timely data sharing and embedded clinical insights directly into provider workflows. Through tools like automated EHR alerts, clinicians received real-time notifications that flagged patient-specific considerations, such as potential medication adherence risks or missed follow-up appointments. This capability empowered healthcare providers to proactively close gaps in care and intervene at the most critical moments. By fostering this level of coordination and supporting data-driven interventions, the industry successfully aligned the distinct goals of payers and providers around the shared objective of improving patient outcomes while effectively managing costs, marking the transition of RWE from a promising concept to a foundational element of modern healthcare.