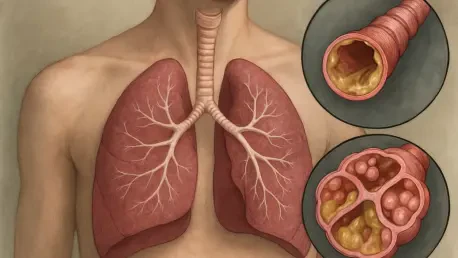
In a groundbreaking stride toward transforming healthcare for individuals with cystic fibrosis (CF), a genetic disorder impacting the lungs and digestive system through sticky mucus buildup that complicates breathing and nutrient absorption, a team from Exeter has spearheaded an innovative approach using wearable technology. This initiative, driven by cutting-edge research, seeks to revolutionize how physical activity is monitored and integrated into the daily lives of those with CF. With the condition often leading to significant health challenges, the need for precise, data-driven solutions has never been more critical. The updated guidance from a leading European society, shaped by this Exeter-based team, marks a pivotal shift after a decade, advocating for advanced tools like fitness trackers and smartwatches to capture comprehensive activity data. This development promises not only to enhance patient care but also to reshape clinical research by providing deeper insights into daily routines and health outcomes.
Revolutionizing Activity Monitoring with Wearable Tech
The core of this transformative guidance, led by Professor Craig Williams from the University of Exeter Medical School, centers on adopting a standardized, technology-driven method to track physical activity in CF patients. Wearable devices, such as sensor-equipped clothing and smartwatches, are recommended to record a full 24-hour spectrum of activity, encompassing everything from light movements to vigorous exercise, as well as sedentary periods and sleep patterns. Unlike older tools like basic pedometers, these modern devices capture data in short intervals—often as brief as one second—offering a level of precision that was previously unattainable. This holistic approach aims to provide clinicians and researchers with a clearer, more accurate picture of a patient’s lifestyle, enabling tailored interventions that can significantly improve health management. The shift to such technology represents a departure from less reliable methods, setting a new benchmark for how activity data is gathered and utilized in care plans.
Another vital aspect of this initiative is the recognition of wearable tech’s potential to bridge gaps in traditional monitoring practices. While self-reported questionnaires and activity diaries still hold some value for capturing personal context, they are now viewed as supplementary rather than primary tools due to their subjective nature and potential for inaccuracy. The expert panel behind the guidance emphasizes that the detailed, real-time data provided by wearables offers a far superior foundation for both clinical decision-making and research studies. This move toward objectivity addresses long-standing challenges in comparing health outcomes across different populations and studies. By focusing on consistent, measurable data, the Exeter team’s recommendations pave the way for more personalized care strategies, ensuring that individuals with CF receive support that aligns closely with their unique activity patterns and needs.
Addressing Gaps in Research and Care Standards
One of the most pressing issues highlighted by the Exeter-led team is the historical inconsistency in how physical activity is measured among CF patients, a problem that has hindered the ability to draw meaningful comparisons or assess long-term health impacts. After reviewing nearly 7,500 studies, with 90 identified as particularly relevant, the panel found that varying methodologies have created significant barriers to progress. The new guidance seeks to resolve this by advocating for standardized protocols using wearable technology, which can deliver uniform data across diverse settings. Co-chairs of the associated working group, Dr. Don Urquhart and Dr. Thomas Radtke, describe this as a timely consolidation of evidence, reflecting a collective effort to better understand how activity influences critical health metrics like hospital admissions and survival rates. This focus on standardization is seen as a crucial step toward improving both individual outcomes and broader research reliability.
Beyond measurement challenges, the guidance also underscores the growing importance of physical activity as a cornerstone of CF management, particularly as advancements in treatment have extended life expectancy for many patients. Exercise is increasingly recognized for its role in enhancing respiratory function, preserving muscle strength, and supporting mental well-being. However, the absence of a unified international or national standard for the type and amount of activity suitable for CF patients remains a notable gap. The Exeter team’s work aims to address this by embedding physical activity as a regular, evidence-based component of care. The ultimate goal is to foster longer, healthier lives through structured, technology-supported exercise plans that can be adapted to each patient’s condition and lifestyle, ensuring that the benefits of activity are maximized in a safe and sustainable way.
Building a Foundation for Future Health Innovations
Reflecting on the strides made by the Exeter team, it’s evident that their leadership in integrating wearable technology into CF care marked a significant turning point. Their efforts established a robust framework that prioritized precision and standardization over outdated, inconsistent methods. By championing devices that captured real-time, detailed activity data, the initiative laid crucial groundwork for enhancing patient care through personalized exercise strategies. The comprehensive review of global research that informed this guidance ensured that the recommendations were rooted in solid evidence, addressing systemic challenges in health outcome assessments with clarity and purpose.
Looking ahead, the focus shifts to actionable steps that can build on this foundation. The next phase involves further studies to solidify the links between specific activity levels and clinical outcomes, ensuring that wearable tech’s full potential is realized. Collaboration among international health bodies is encouraged to develop unified standards for activity recommendations, while clinicians are urged to integrate these tools into routine care. This Exeter-led effort not only redefines monitoring practices but also sets a clear path for future innovations, promising a healthier, more active future for those living with CF through sustained, evidence-driven progress.