For decades, radiation therapy has stood as a formidable pillar in the fight against cancer, yet its application has often resembled a powerful but imprecise tool, creating a critical need for a more refined approach. The very playbook that has guided oncology is now being re-evaluated, as new technologies promise a future where treatment is tailored not just to a type of cancer, but to the intricate clinical and biological profile of each individual patient. This shift marks a pivotal moment in the evolution of cancer care, moving from broad-stroke protocols toward hyper-personalized intervention.
Rewriting the Standardized Playbook for Cancer
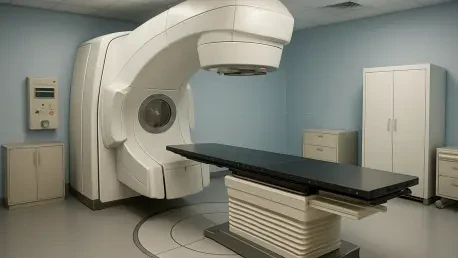
Radiation therapy has long been a cornerstone of cancer treatment, effectively destroying malignant cells and shrinking tumors. However, its traditional application has been based on generalized protocols that treat cancers of a certain type and stage in a largely uniform manner. This methodology, while effective to a degree, does not fully account for the vast variability between patients, from their genetic makeup to their specific anatomical nuances.
The emerging paradigm in oncology is one of deep personalization, powered by data and artificial intelligence. The goal is to create a treatment plan that is as unique as the patient receiving it. By integrating a patient’s complete medical history, genomic data, and advanced imaging, AI can identify patterns and predict outcomes with a level of detail that was previously unattainable, setting the stage for a new standard of care.
The Urgent Need for Precision Beyond One Size Fits All
The fundamental limitation of conventional radiation therapy lies in its potential for collateral damage. High-energy beams powerful enough to eradicate a tumor can also harm the healthy tissues and organs surrounding it, leading to a range of side effects that can impact a patient’s long-term quality of life. This creates a constant and delicate balancing act for clinicians.
Oncologists are perpetually faced with the challenge of delivering a radiation dose aggressive enough to control the cancer while minimizing harm to the patient. This tightrope walk between efficacy and safety underscores the urgent need for greater precision. A more targeted approach would not only improve treatment outcomes but also significantly reduce the risk of debilitating side effects, a crucial consideration in survivorship.
Gemini RT A New Alliance Forging the Future of Oncology
In response to this challenge, a strategic collaboration between GE HealthCare and Mayo Clinic has been established to fundamentally reshape cancer care. This initiative, known as GEMINI-RT, aims to integrate three core technologies: advanced imaging, artificial intelligence, and sophisticated patient monitoring to create a seamless, data-driven treatment ecosystem.
The initiative overhauls the treatment planning phase by using AI to analyze a patient’s full medical history alongside vast datasets from thousands of similar cases. This allows clinicians to calculate an optimal, individualized radiation dose that maximizes tumor destruction while sparing healthy tissue. Furthermore, connected care tools are employed during and after treatment to monitor vital metrics like heart rhythm, enabling the pre-emptive identification of potential side effects such as cardiotoxicity and allowing for immediate clinical intervention.
The Expert Vision From a Standard Model to a Precision Method
The core objective of the initiative is a decisive shift in treatment philosophy. As articulated by Ben Newton, GE HealthCare’s global head of oncology, the goal is to evolve radiation therapy “from a ‘one-size-fits-all’ model to a precision-based method.” This vision is not just aspirational; it is grounded in a robust and credible partnership.
This new venture builds upon a prior radiology research agreement, cementing a history of successful collaboration between the two institutions. With all research activities anchored at Mayo Clinic’s world-renowned campus in Rochester, Minnesota, the initiative leverages a deep well of clinical expertise and technological innovation, lending significant weight to its ambitious goals.
The Roadmap from Innovative Research to Global Patient Access
The collaboration is structured around a five-year strategy designed to translate cutting-edge research into tangible clinical practice. The roadmap includes launching new clinical trials to validate these personalized approaches, conducting retrospective studies to mine historical data for new insights, and evaluating novel technologies that can further enhance treatment precision.
Beyond refining existing methods, the initiative is also exploring the next frontier of oncology: innovative combination therapies. The research will investigate how personalized radiation can be paired with other emerging treatments, such as targeted drugs and precision heating, to create synergistic effects. The ultimate vision is to integrate these proven innovations into GE HealthCare’s global product portfolio, ensuring that advanced, personalized cancer care becomes accessible to patients and clinics worldwide.
The launch of this ambitious collaboration marked a significant step toward a new era in oncology. It represented a departure from generalized protocols and a committed move toward a future where cancer treatment was defined by individual patient data. The initiative aimed not just to improve an existing therapy but to fundamentally reconstruct its delivery, ensuring that every patient received a plan optimized for their unique biology, which promised to enhance efficacy and redefine patient safety for years to come.